And eligibility screening for Case Management is required only every three years and is valid for three years.
Persons with SPMI (Serious and Persistent Mental Illness) are eligible for case management. A "person with serious and persistent mental illness" means an adult who has a mental illness and meets at least one of the following criteria:
Use the following flowchart to determine eligibility for Case Management services:
For a client without a current DA who declines to participate in a DA, services may begin with an eligibility screening based on records available, interview with the client, and other sources, including the referral source. For presumptive eligibility all of the following conditions must be met:
Ask your Program Manager for permission to initiate AMH-TCM services for residents of other than Lake and St. Louis Counties.
We do not provide AMH-TCM services to residents of Carlton County without prior notification to Carlton County.
Lake County referrals should come from Lake County only. Direct 3rd parties to Lake County, instructing them to send the request and Diagnostic Assessment to Lake County for eligibility screening and a referral.
If our Diagnostic Assessment recommends new Case Management services for a Lake County resident, we should do the same.
When we receive a referral and complete an eligibility screening for a resident of St. Louis County, who also has straight Medical Assistance (non-PMAP/non-MCO) insurance, please complete the following document and send it to St. Louis County:
It is not necessary to complete this form for a client who begins services on a PMAP and then loses coverage temporarily. Only for those clients who first initiate services in St. Louis County on straight Medical Assistance.
It is strongly recommended that you fill out this form entirely on your laptop to the point where it is ready for signatures. (It's just easier.) Then email it to yourself and use the signing part of the instructions for using it on the iPad below to have your client sign it. But you You can fill out the entire form, and get signatures on an iPad or phone as follows:
When a current client moves to a new county where we can no longer provide Case Management Services, you may continue to provide these services for up to 60 days, or until you have connected them with a provider in their new county-of-residence, whichever comes first. If we have a presence in the new county-of-residence, referral and transfer to BHH services is also an option.
Explain this, and then explain options. Give the individual a list of Case Management providers in their county of residence and offer to make a referral, or offer BHH services as an alternative if the individual does not want to change providers.
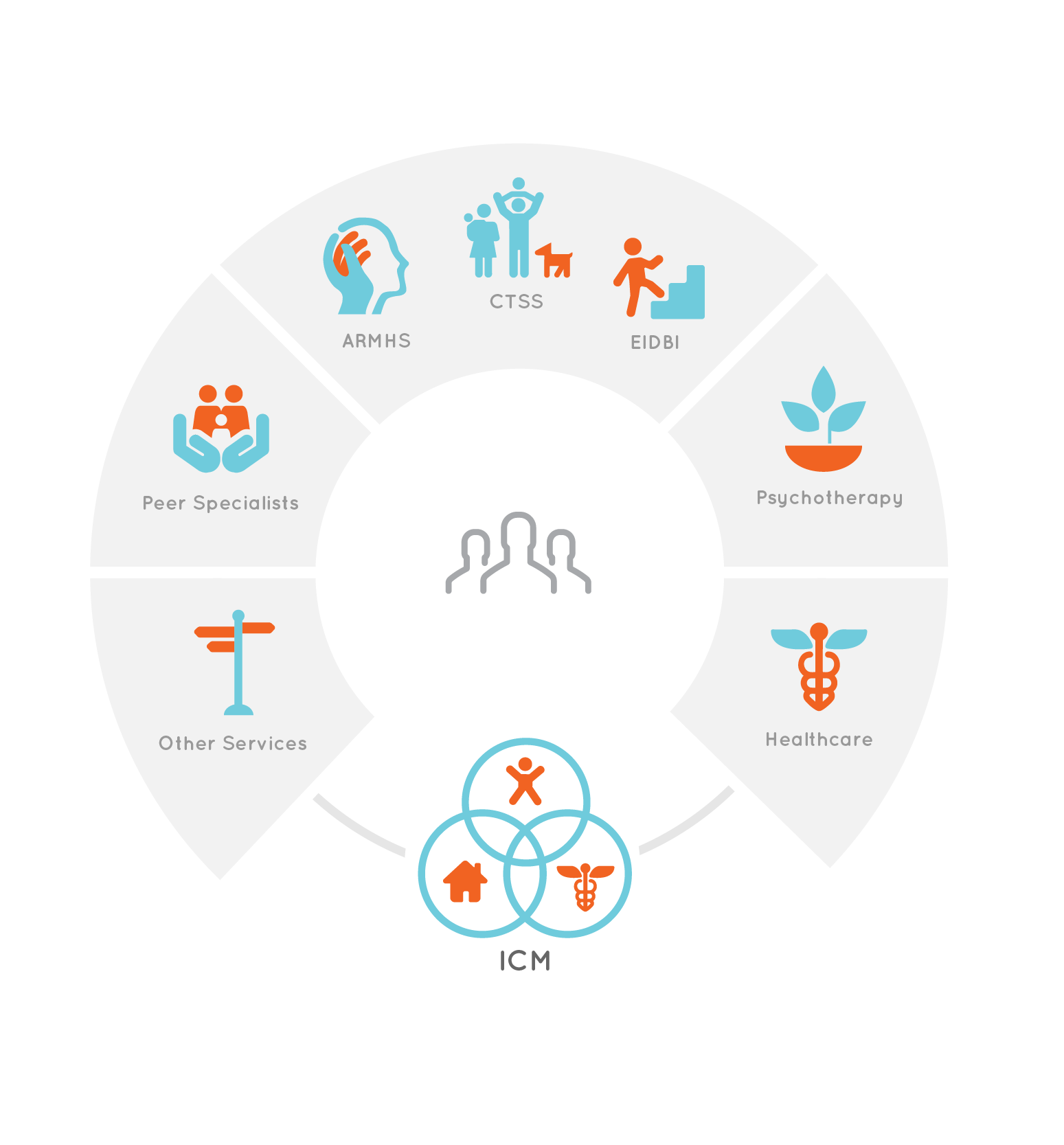
Assessment, Planning, Progress Review, Monitoring Quality and Coordinating services are the key core elements of Integrated Care Management. This is not paperwork or a compliance exercise. It is the core responsiblity and activity of high quality Integrated Care Management. By doing this important work, Integrated Care Managers make possible, enhance, and assure coordination of all of the other services we provide and integrate these services with other health care, mental health, residential, vocational support, and social services.
While not specifically described in the diagram here, as one of the four core services, helping the individual's you serve with maintaining health care coverage is essential, because without it, they cannot receive the medically necessary services to which you will refer them. A large number of the people to whom we provide Integrated CareManagement services see their insurance lapse for many reasons, but most often because they do not complete eligibility renewal applications and required verifications on time when their annual renewal is due. Read more about the steps you should take to monitor and help individuals with eligibility renewal under the topic Insurance Advocacy in the Advocacy section of this guide.
Our referrals most often come to us because they have immediate unmet basic needs. These might be financial, housing, food, safety, health care, or other unmet needs. While assessment and service planning is an important first process in developing and delivering Integrated CareManagement services, it should be done in the context of meeting immediate needs. Helping your client to identify resources and get these needs met is an ideal opportunity to learn about what has led to their current status, as well as what strengths and resources they have that will help them better meet needs and avoid these crises in the future.
Assessment is the first priority in Integrated Care Management, but high quality assessment is much more than completing the document. It is a dynamic process used to identify current strengths and resources, needs, and deficits, and to prioritize these into Integrated Care Plans, Action Lists, and Referrals. It is not a process that occurs just once every 6 months, either. It is ongoing. The time to begin on the update to any assessment is the day after you have completed the previous one.
The Health Care and Other Referrals and Action Lists are tools meant to be used, not as a compliance exercise, but as a to-do list to ensure that a recipient's healthcare and mental health needs are being met. For each client, develop a specific Action List and Referrals List based on their specific needs should inform priorities.
Our payers have also asked us to develop processes to assure quality care in a variety of specific ways. What follows are examples of items that UCare has asked included in Action Lists. While not a comprehensive list, it highlights some key areas on which we should focus for all clients.
- Annual Wellness Visit – Clients schedule and receive their annual medical wellness visit.
- Dental- Clients schedule and receive their annual dental exam
- Antidepressant Medication Management – Clients who are prescribed an antidepressant medication and continuously fill their medication for at least 180 days (6 months).
- Diabetes screening for people with Schizophrenia or Bipolar Disorder – Clients who have a diagnosis for schizophrenia, schizoaffective or bipolar disorder and are prescribed an antipsychotic received a screening for diabetes. Screening would be a A1c test result.
- Diabetes Care - Clients who are diagnosed with diabetes (type 1 or type 2) and had the following screens:
- Eye exam performed (to check for diabetic retinopathy)
- Hemoglobin A1c (HbAIc testing)
- P control (optimal is <140/90 mmHG)
- Medical attention for nephropathy (a urine test for albumin or protein in urine)
You can also find additional suggestions for action items on this checklist published by the Minnesot 10x10 initiative for Improving Health for Persons with Bipolar Disorder or Schizophrenia. Read more about the Minnesota 10 by 10 Initiative: Healthier, longer lives for people with mental illness here.

Integrated Care Planning
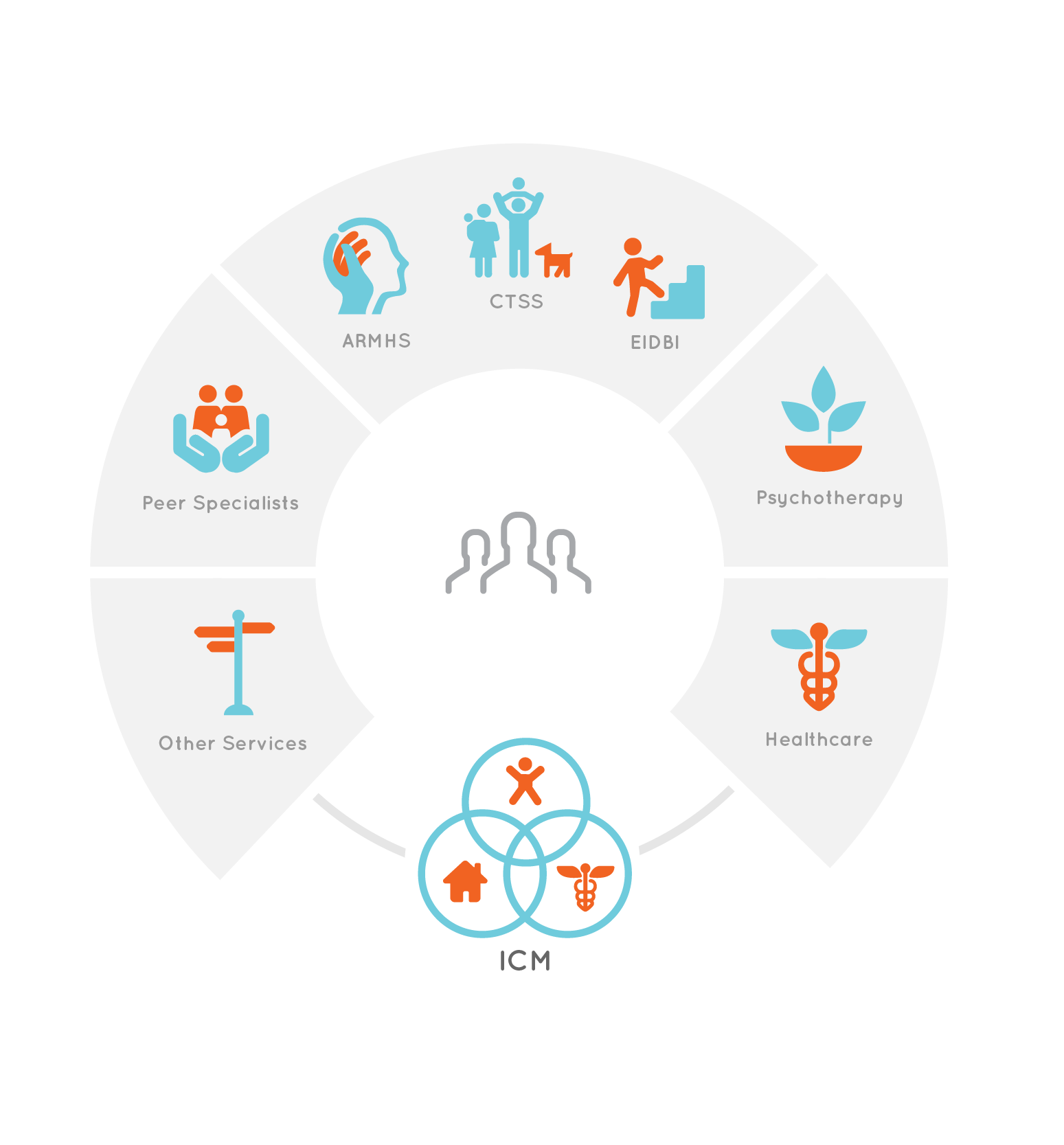
The Integrated Care Plan brings together all services individuals receive from Accend into one integrated plan. (And exception to this is children who received EIDBI services - EIDBI plans, being more complex, are kept separate.)
It is the Integrated Care Manager's primary duty to complete or facilitate completion of all necessary assessments, and facilitate the development of an Integrated Plan.
Complete the Integrated Care Plan following these steps and guidelines:
- During the intake interview, and subsequent follow-up sessions, you are likely to ask, "What brought you here?" or something similar. The individual might answer by identifying needs. Using the TabsTM Long-Term Goals utility, complete a list of the individual's long-term goals by reframing these needs statements into positive accomplishments, describing the individual's goals, hopes and dreams. Label each of these goals as a Personal Goal, Treatment Goal, or Recovery Vision.
- For each long-term goal, identify the first steps the individual might take to achieve them and what supports and other services he or she needs. These are Objectives. Record them in the TabsTM Manage Objectives utility.
- The Case Management or Behavioral Health Home Objectives in the should be characterized by the four core elements of Integrated Care Management services.
- Objectives for all services in the Integrated Plan should also be tangible and measurable. They describe accomplishments, changes in habits or behavior, and obtaining and participating in medically-necessary health and mental health care, residential, educational and vocational supports and other social services.
For more information about writing person-centered Long-Term Goals and measurable Integrated Care Plan Objectives, see the section on Assessment and Planning in this guide.

Referral and Linkage
Referral and linkage involves interactions with the recipient to:
- connect the recipient with informal natural supports;
- link the recipient with the local community, resources, and service providers;
- refer the recipient to available health and mental health treatment and rehabilitation services;
- assure that individuals receive regular recommended well care, and treatment of health conditions
- learning about and understanding the person’s culture, individual preferences and communication needs, identifying resources to meet his or her needs, and cultivating relationships with other community and social support providers to aid in effective referrals and timely access to services.
- where available, refer to Peer Support Services to improve engagement and strengthen relationships based on a shared affiliation and a deep understanding of this experience. In self-help and mutual support, people offer this support, strength, and hope to their peers, which allows for personal growth, wellness promotion, and recovery.
Referring an individual to services does not stop with the phone call, fax, or referral form. Integrated Managers identify, with high quality assessment, what barriers might exist for an individual to participate in recommended services. Can they get to the service? Do they have transportation? Do symptoms, such as depression, anxiety, or phobias prevent them from participating? Do they have children who may need childcare while they participate in services? These are just a few considerations that the thoughtful Integrate Care Manager must take into account when making referrals, and address with a comprehensive Integrated Care Plan that removes these and other barriers to participation.
Monitoring and Coordination
Once you have identified needs, made referrals, and an individual is participating in services, monitoring and coordination of the services is the primary role of the Integrated Care Manager and serves these purposes:
-
Reviewing programs and services for accountability, assuring that everyone is addressing the same purposes stated in the Integrated Care Plan so that the recipient is not exposed to discontinuous or conflicting interventions and services.
- Determining if goals and objectives in the Integrated Care Plan are being achieved according to the Integrated Care Plan’s projected timeline(s) and that they continue to fit the recipient’s needs.
- Identifying barriers to participation and connecting individuals to additional resources they need to maintain successful participation.
- Monitoring service and support outcomes through ongoing observations, making changes in the Integrated Care Plan and recommending changes in service plans for other services when goals are achieved or progress is slow or stalled.
- Assuring that care is well-coordinated between various health and mental health/behavioral health care providers.
- Identifying emerging new needs by staying in touch with the recipient to identify problems, modify plans, and ensuring that the recipient has resources to participate in services and accomplish goals.
- Coaching and education about health and wellness to increase self-efficacy, improve health management, maintain a healthy lifestyle and improve health outcomes. Where applicable this includes family and caregiver education.
- When individuals are hospitalized or placed in residential care creating a plan to follow after the person’s discharge from hospitals, residential treatment and other settings, maintaining contact between the BHH services team member(s) and the person and his or her identified supports during and after discharge, and linking people to new resources as needed.
Facilitating Recovery Team Meetings
At regular intervals associated with treatment/service planning updates, Integrated Care Manager Managers should offer to each person served an opportunity for a Recovery Team Meeting. The purpose of the Recovery Team Meeting is to bring together all providers and other key natural support persons chosen by the individual to review progress, set new goals, and further define each person's health and recovery vision.
The Integrated Care Manager assigned to each person served should offer and facilitate this process if that individual chooses.
Coordinating Internal Services
At Accend, we organize ourselves using the strategy of Integrated Teams. This means that, as much as possible, when our clients receive more that one service from us we refer our clients to providers on the same team where they receive Integrated Care Management tservices. This is not always possible. At times, there are providers, psychotherapists for example, who are members of a different team, but who have particular specialties that are a better fit for the individual's needs.
Regardless of whom the individual's providers are for other services they receive at Accend, Integrated CareManagers are tasked with coordinating these services, assuring that where, for example, a recipient of Integrated Care Management also receives ARMHS, the ARMHS plan is coordinated with and supports the goals and objectives in the Integrated Care Plan.
When a recipient of Integrated Care Management also receives Psychotherapy services, the Integrated Care Manager works hand in hand with the therapist to ensure that Psychotherapy services are responsive to needs, and that Integrated Care Management (and other services, such as ARMHS or CTSS) support the goals and objectives of Psychotherapy.
Finally, for all services, the Integrated Care Manager assures that individuals other basic needs are met so that mental health treatment can be as effective as possible.
Monitoring Internal Services Using TabsTM
When recipients' receive other services at Accend, follow these steps to assure engagement, quality and effectiveness of these services:
- At least twice monthly, use the Client Time Report in TabsTM as shown in the image below to view the services the recipient has received and is scheduled to receive.

- Open the recipient's electronic file, navigate to Schedules and Reports, and select Client Time Report.
- Select a date range. The range may include future dates to view scheduled services.
- Examine the report to see that the recipient is receiving planned services.
- Where there are frequent cancellations, disengagement, or other reasons why the recipient has not received planned services, follow up with the recipient and other providers immediately.
Coordinating With Other Services
For recipients receiving other services, coordinate communication with the full team to review progress and engagement in services:
- each time assessments and the Integrated Care Plan are updated;
- at any time engagement or progress in any service appears stalled;
- when the recipient experiences a substantial change in status (residence, employment, family, or other), or following significant health care or mental health events; or
- at any time substantial progress indicates that modifications to the plan might be warranted.
When functioning is a barrier to goals, the Integrated Care Plan spells out the longer-term, or ultimate, goals and outcomes, and connects the recipient to supports to remove functional barriers. For recipients who receive other services, the Integrated Care Manager must ensure that the Plan is coordinated, and demonstrates clearly how each service will support the goals and objectives in it.
When recipients disengage from Integrated Care Management services but remain connected to other services, coordinate with those providers to explore the reasons why the recipient has disengaged.


Best Practices for Proactive Contact
Having phone or face-to-face contact with all Integrated Care Management Services recipients in the first 10 business days of each month provides an opportunity to triage needs, plan, and prioritize for the remainder of the month. To do this:
- Schedule a repeating appointment with all clients in the first 10 days of each month
- If any client is inconsistent in attending these appointments, call first to confirm before traveling to the appointment
- Always, while contact and scheduling, if you reach and individual, conduct a brief assessment (triage) of their needs over the phone and document this as Phone Contact. Schedule a follow-up on identified needs for later in the month.
- If an individual does not attend an appointment, document using the add-on Contact and Scheduling Following CCN within the Client-Initiated Cancellation Note.
- If you do not have contact with any individual, continue to make and document at least two more efforts to contact them in the first 10 business days of the month.
- Minimum necessary effort in this practice is at least three efforts to contact in the first 10 business days (one cancellation and two additional efforts to contact them).
When you are unable to reach an individual for a protracted period of time, make these additional efforts:
- Are they engaged in other services at Accend? If so, Use the custom time report to view scheduled appointments in the future and connect with those providers and facilitate contact (perhaps during their next appointment).
- Do they have a referral source or other contact person you may contact (with permission) to try to locate and contact them? Document this contact as Contact and Scheduling.
Contact Expectations
Frequency of contact is person-centered, but expectations for minimum contact with individuals receiving Integrated Care management services are as follows:
- Each Integrated Care Manager contacts every active client within the first ten working days of the month to review progress from the previous month, assess needs and plan for services in the balance of the current month. This may be a telephone or face-to-face contact, as long as the service provided is one of the core Integrated Care Management services.
- Each recipient receives at least follow-up visit to carry out the monthly plan, or as many as necessary to meet needs.
- Integrated Care Managers respond immediately to urgent needs (circumstances that threaten health, safety or the individual's ability to meet basic needs.)
- Integrated Care managers make a minimum of one meaningful effort per week to contact individuals who have disengaged.
These efforts can include contacting other providers or collateral contacts for whom we have written permission to communicate, until such time as the decision is made to place the individual in closing status because we are unable to contact them.
Minimum contact for Integrated Care services are as follows:
- Face-to-Face or telephone contact every calendar month
- For AMH-TCM, face-to-face (or audio+visual telehealth) contact no less often than every three months
- For BHH, face-to-face (or audio+visual telehealth) contact no less often than every six months
These are minimum standards. Best practices are a telephone or face-to-face contact in the first ten business days every month to review progress and assess needs, and follow-ups as needed throughout the month, with face-to-face contact every month begin the preferred standard.
Use Advanced Searches
Tap here for a tutorial (ICM My Efforts Report) on how to use and Advanced search to track your contacts and contact efforts with Case Management and Behavioral Health Home Services clients.
Procedures for Prolonged Lack of Face-to-Face Contact
In Case Management, if you have had only telephone contact with an individual by phone during the previous two months,you must have face-to-face contact that month for the service to be billable. BHH phone contacts are acceptable for 5 months before a face-to-face contact is necessary.
Contact With Identified Supports - BHH
For Behavioral Health Home services, specifically, contact with identified supports. An identified support is anyone named by the person receiving services as someone who can be in communication with the BHH services team to support them in meetings their health goals.
Identified suppports may include non-guardian relatives, advocates, housemates, school personnel, housing support workers, or other key support persons identified by the recipient or guardian.
The following must occur once the person receiving BHH services has named their identified support(s):
- Describe the identified support(s) in the member’s health action plan in the Recovery Team Members element
- Complete a release of information form for each identified support
- Document this type of contact with the note type xBHH Contact with Identified Supports
- This contact is considered a billable contact type for BHH services even if it is the only contact provided in a given month.

Working with recipients to assure that they receive routine well-care and treatment for physical health conditions is a priority in Integrated CareManagement services. Providing support as needed to each individual to maintain health care coverage is the first step in this process.
Regardless of whether or not each recipient has significant health problem, monitor and record health care in TabTMas follows.
- Record all current health care providers in client Info > contacts. This is a necessary first step, as subsequent steps will require you to select providers from the contact persons list.
- Ask individuals to sign Releases of Information to receive health care and other records from providers.
- Record health needs and health problems in health care and other referrrals > action List.
(Include well care, annual physical exams and twice dental cleaning and exams in each person's list.)
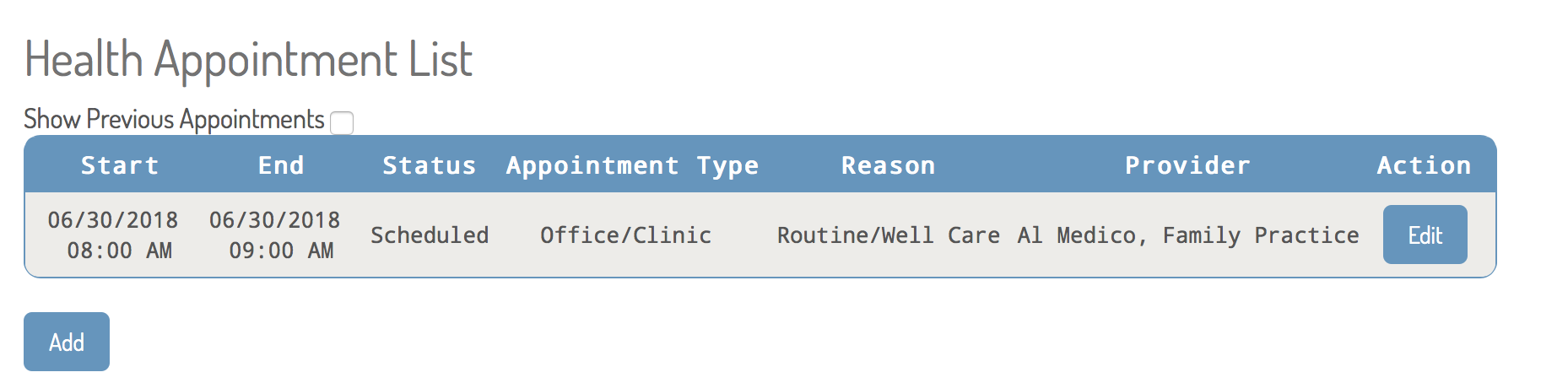
- Track appointments made and attended in health care and other referrrals > appointments.
- Track prescriptions and medications in health care and other referrrals > medications.
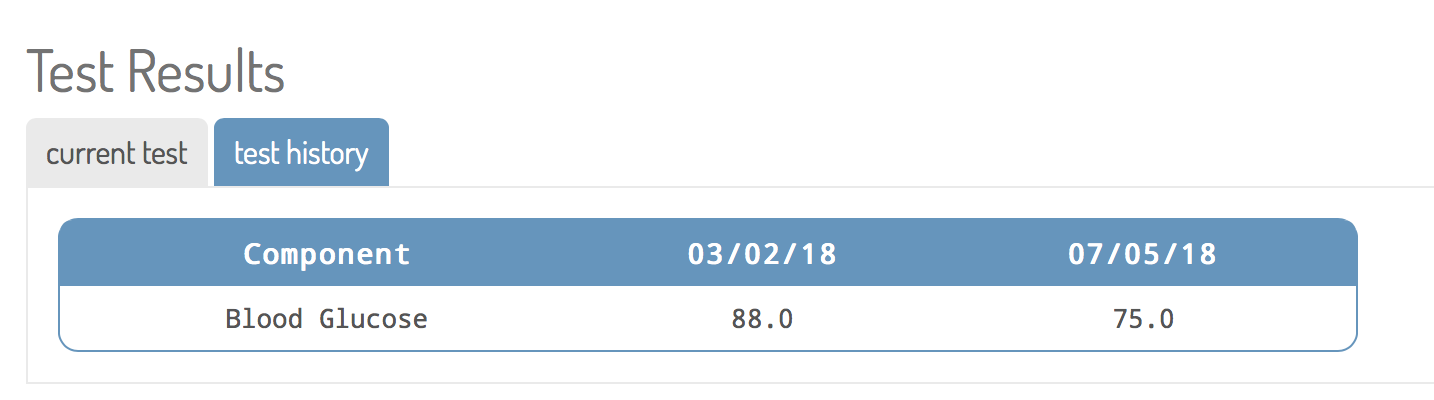
- Record lab results from health care appointments, if applicable, in health care and other referrrals > labs.
- Where applicable track immunizations in health care and other referrrals > imunizations.
As needed, develop person-centered goals and objectives for improving each individual's health and access to and management health care services in the Integrated Plan. Seek advice from the Accend RN, and each person's physician for goals and objectives involving such things as special diets, exercise, herbals or supplements, especially for individuals who have serious health conditions such as low or high weight, diabetes, high blood pressure, etc.
Well Care, Immunizations and Recommended Health Screenings
A key component of your job as a Behavioral Health Home provider is to educate the people you support about recommended well care, including annual exams, immunizations, and other recommended health care screenings for persons of various ages, backgrounds, and health histories.
Your first task is to connect each person with an ongoing relationship a primary care physician. That physician will make recommendations based on the individual's exams and health histories.
At the same time, you should remain aware of standard recommendations for immunizations and health screenings. Tap on the following links for information about these.

A core strategy of Behavioral Health Home Services is to systematically use a registry to identify specific population subgroups requiring specific levels or types of care. We have developed the following utilities in TabsTM to support this process.
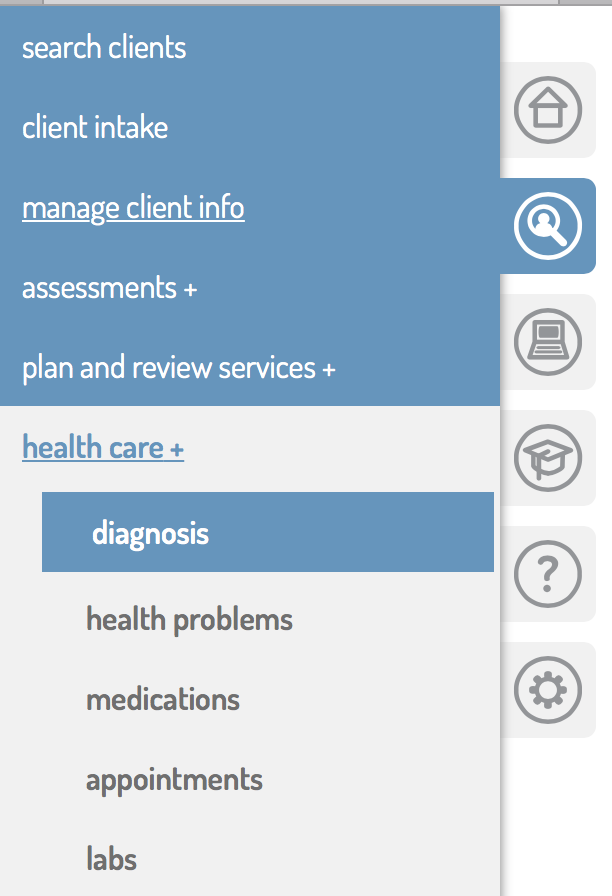
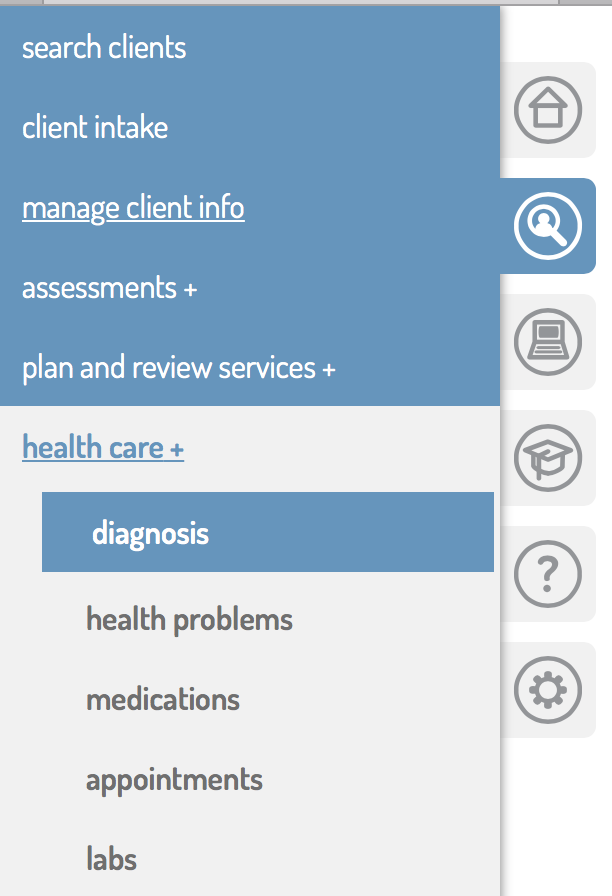
Diagnosis Table
The Diagnosis Table in TabsTM allows for entry of diagnoses received from medical and mental health professionals. To use this tool, select the individual from the search and navigate to diagnoses as shown in the image to the left. From there you may view or add diagnoses to the table.
To use the diagnosis utility:
- Enter the start date, if known, for the diagnosis. For new diagnoses, this is the date it was diagnosed by the medical or mental health professional.
- Enter the ICD10 coded and diagnosis name. For mental heath diagnoses, a lookup utility is availalble. For all other health diagnoses, obtain information from the physician including ICD10 code, date of onset, if known.
- When a health problem is resolved, enter the end date.
- Notify the RN Integration Specialist to review each entry for accuracy.
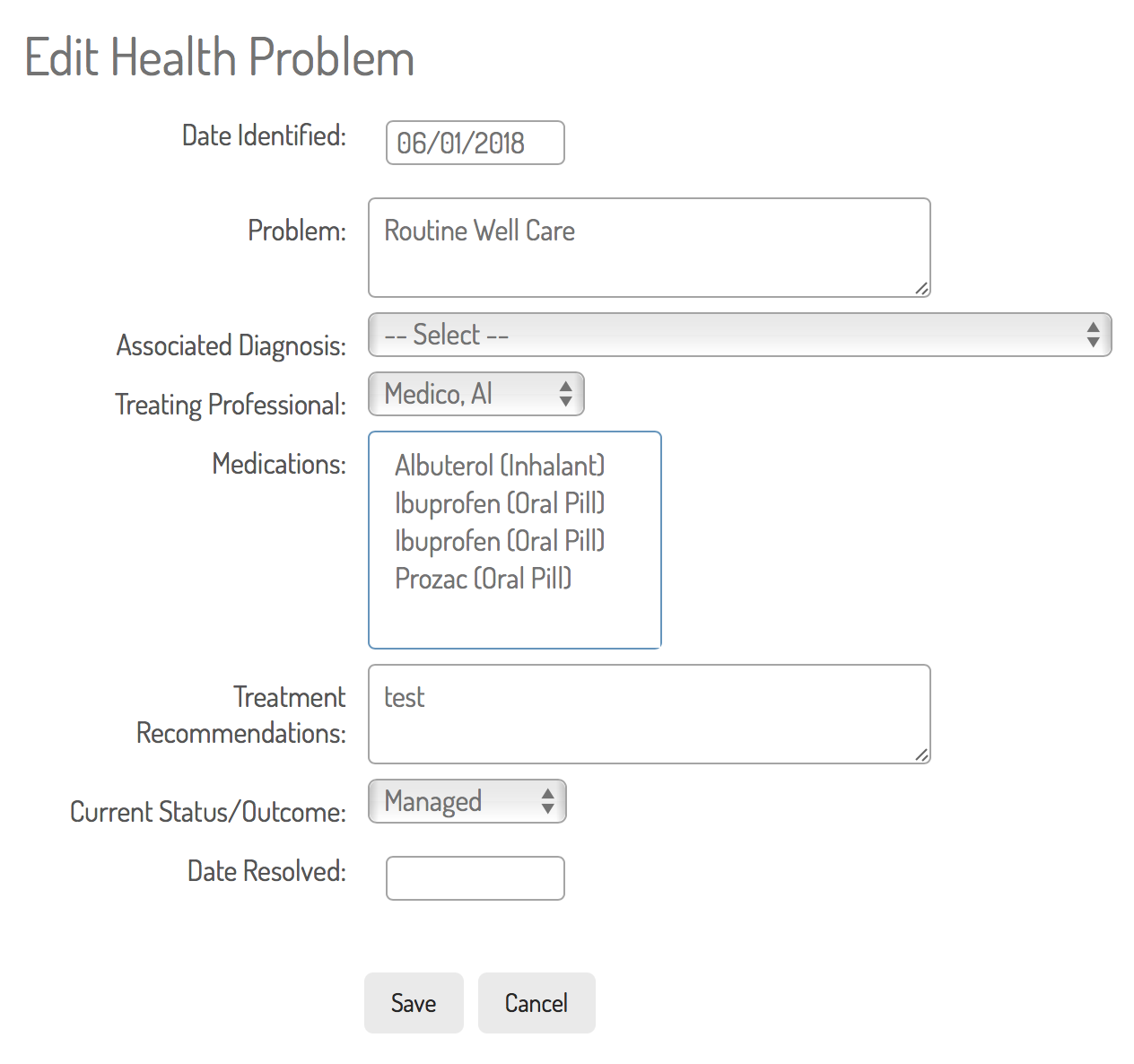
Action Lists
Use Health Action Lists to track health care, social services, housing, vocational and a variety of other needs. For each person served with BHH services, enter well care needs as standard.
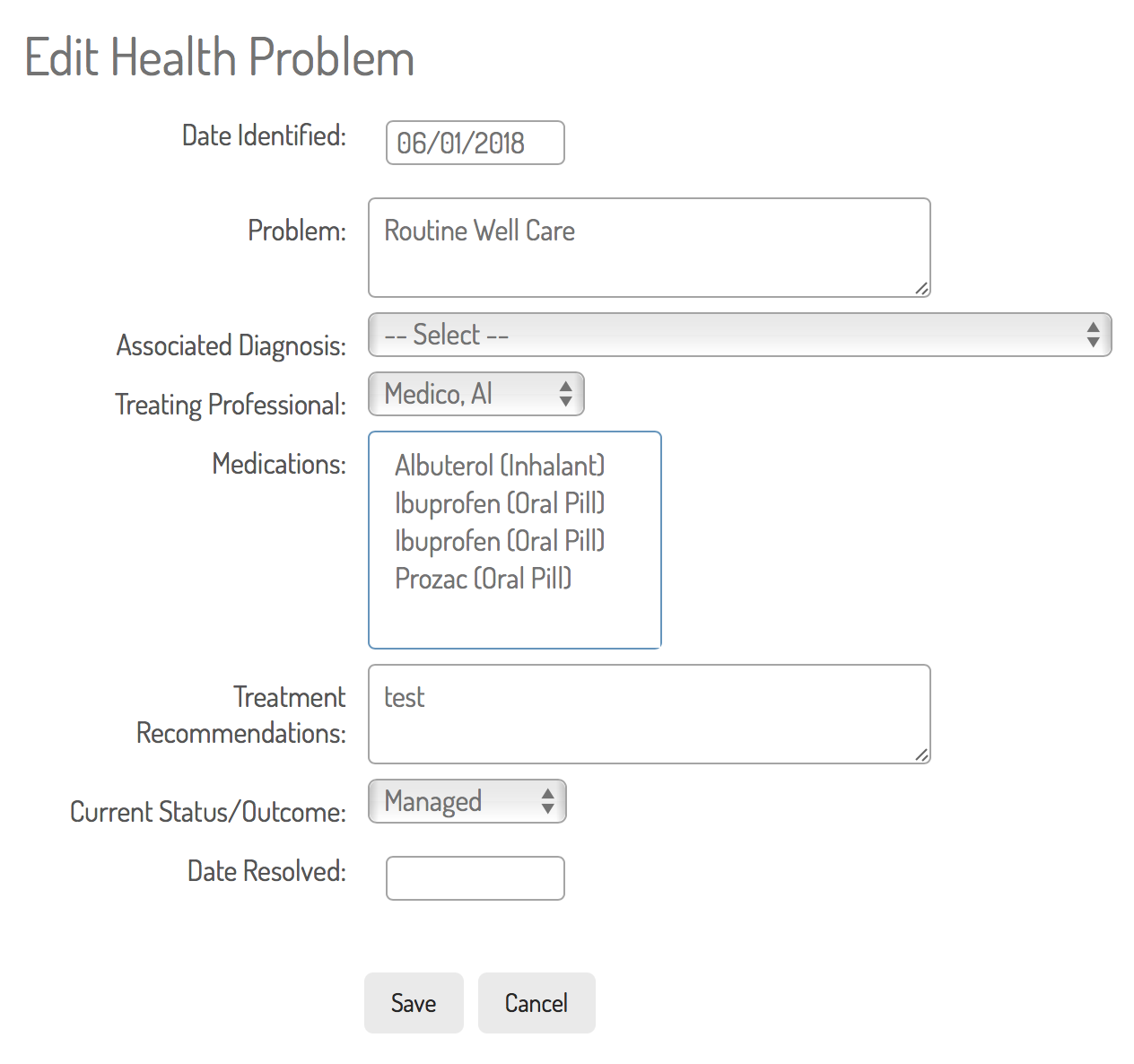
- Navigate to action items in the Health Care and Other referrals menu. View the list of current action items, edit them from the table, or tap to add.
- Enter the date the action item was identified,
- Label the action item using the drop-down list.
- Associate it with a diagnosis if applicable. All of the individual's current diagnoses appear in this drop-down menu. If the associated diagnosis does not appear, you may need to add it to the list using the diagnosis utility.
- Identify the provider if applicable.
- Select from the individual's current list of medications to associate a medication prescribed to treat the health condition, if applicable.
- List additional recomnendations from the provider.
- Identify the current status of the condition, from the drop-down list. if applicable.
- Add a resolution date when the action item is complete/resolved.

Medications Tracking
Track medications in the Medications table as follows:
- Navigate to the Medications list.
- View or edit current or add current new using the Add button.
- Adding a medication offers you a pop-up with a link to standard medications as displayed here. Select the name of the medication from the drop-down and select a strength. Detailed drug information will appear. If this matches the precription information you have recieved, tap add medication in the pop-up window.
- Complete the rest of the form, adding a start date, end date if appplicable, and additional use and dosing instructions.
- Contact the RN Integration Specialist to review the entry.
- Return to the medications list to edit them with end dates as necessary.
- When someone receives doctor's orders for a change in dosage, enter this as a new medication in order to preserve the record of the previous one.
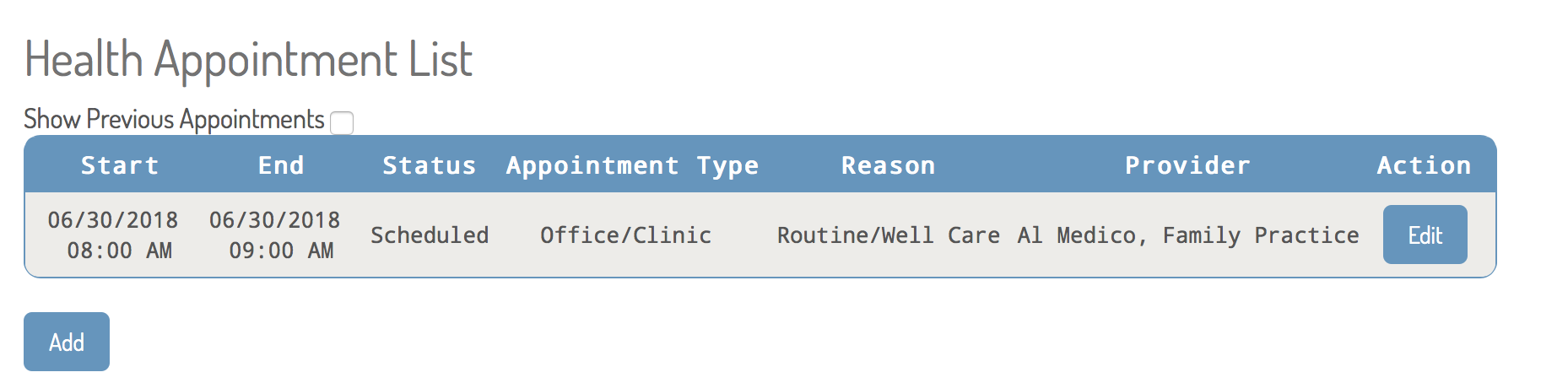
Appointment Tracking
The appointments utility offers you the ability to enter scheduled appointments and then return to enter results. After navigating to this utility, you may tap to edit a current appointment or Add a new one. Fill out the form completely and enter medications changes and lab tests in those utilities as needed.
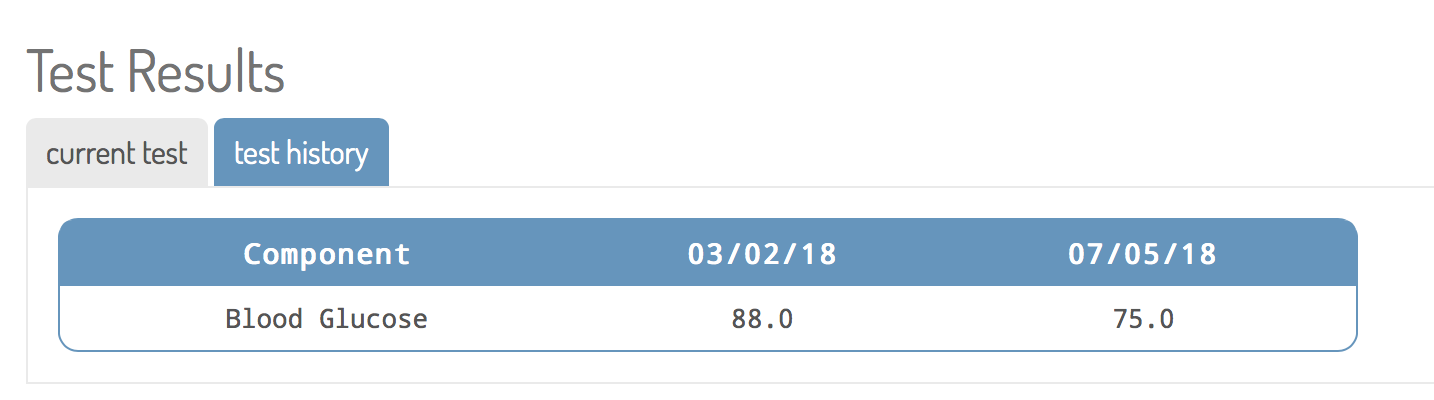
Labs
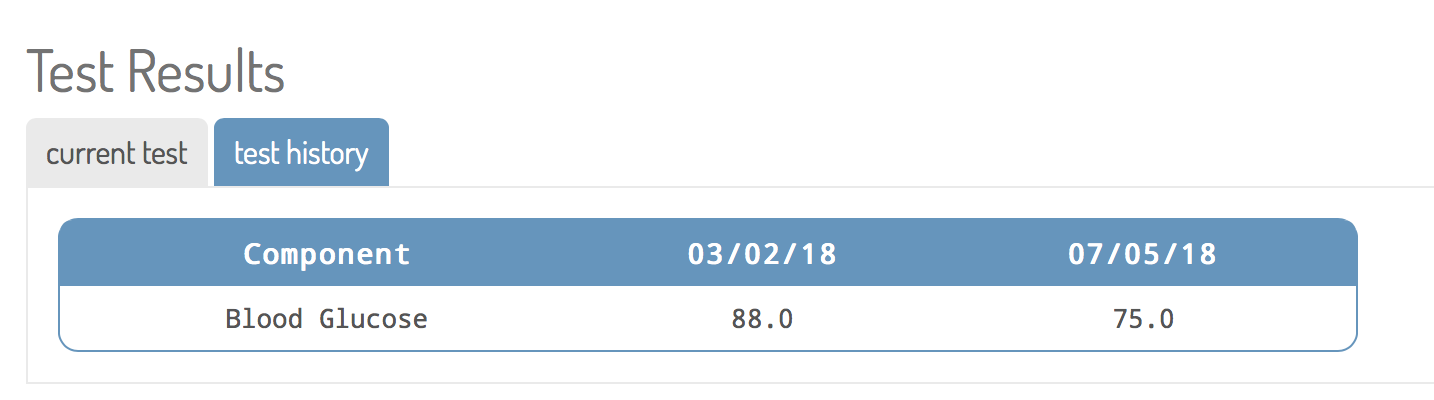
The labs tracking utility is simple to use. Tap on a lab test from the dropdown menu and add it. The labs utility provides a history for each lab test over time, as follows:
Immunizations
The immunizations tracking utility works the same. Tap on an immunization from the dropdown menu and add it.

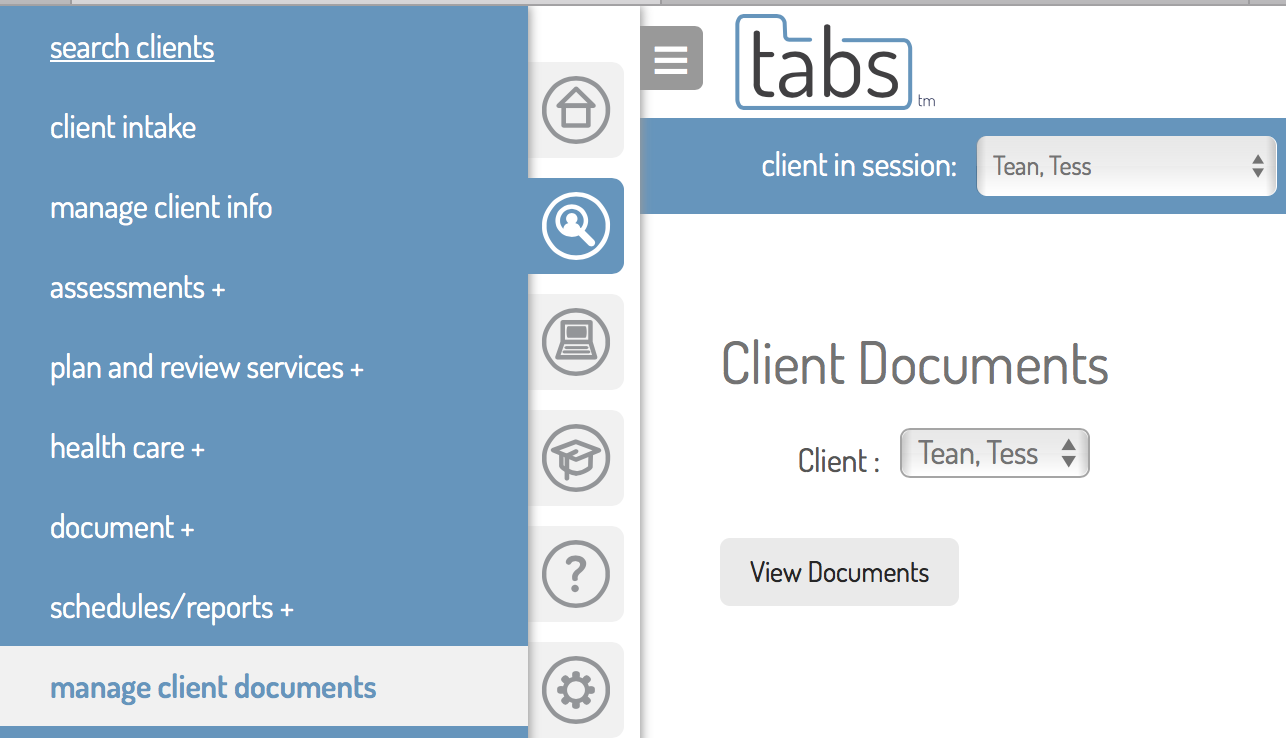
Document Storage
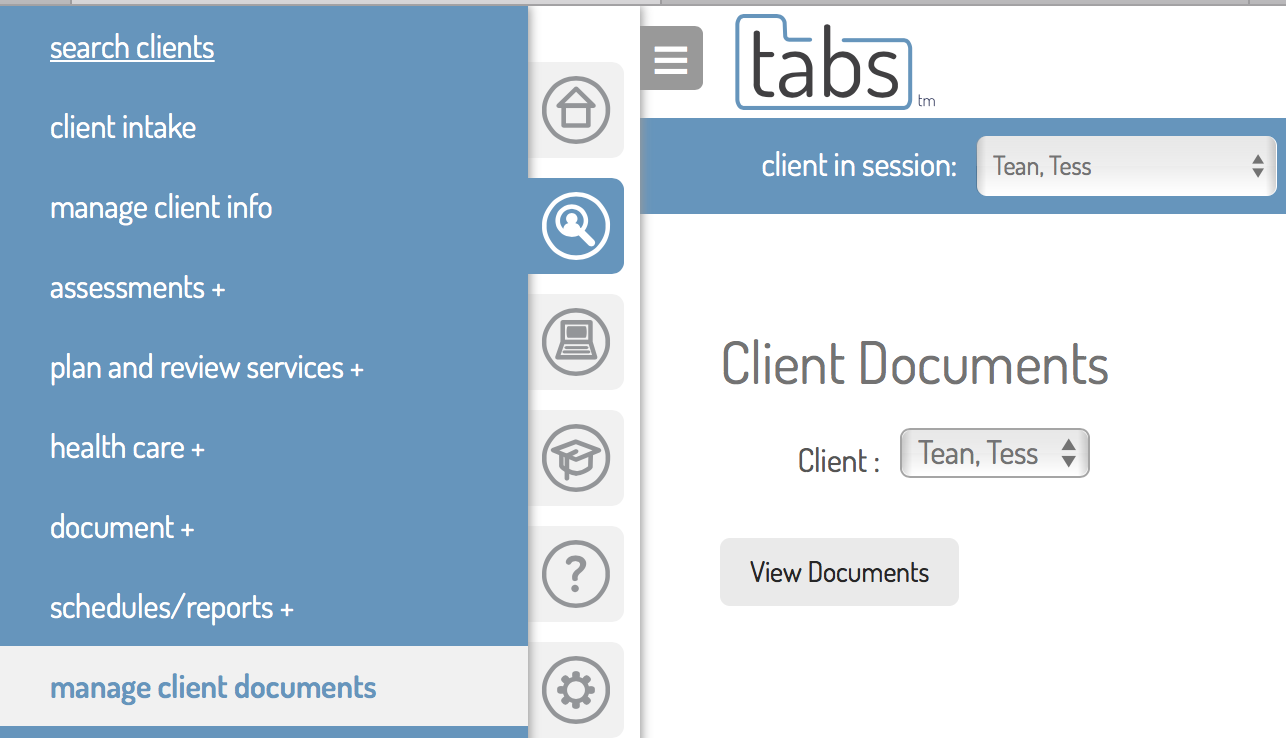
Finally external documents of all kinds can be stored in each person's file. Navigate to documents as shown to the left. Once there, you may view a list of current documents in the file, or add a scanned document. Medical records typically will do this for you, however, if you submit any external or paper document.
Searching the Registry
To search the registry, navigate to Admin Tools, then Audits and Reports. Tap here for a visual guide for using the Registry Search.
Results of the search will appear in a table, which can be reviewed online, or downloaded as a text-delimited file (spreadsheet) for further sorting and analysis.
Using TabsTM to Identify and Manage Care Gaps
TabsTM contains information about immunizations, cancer screenings and disease-specific lab results for the people in your practice. You can search it to identify those persons overdue for annual or other well-care exams, screenings and immunizations and any other well-care services they might need.
You will do this by using the following resources, and the recommendations of each person's physician to create problem lists. These lists, customized to each individual, should identify the well-care, screenings and immunizations they need at this time.
Queries of problem lists can also identify individuals who have specific problems in managing preventative and chronic health care issues. TabsTM queries will help track if each person is meeting these preventive and chronic care measures.
While assisting the people you serve with health care visits, you will prepare in advance and ask physicians and staff to screen the people you support for diseases and for recommended services based on their age, sex, diagnosis, etc. You will remind physicians and providers to provide preventive care services (e.g., immunizations), and help physicians and providers to better manage chronic conditions.
Your Integration Specialist will provide guidance on clinical practice best practices and guidelines for preventive and chronic care services. You will use these to establish target levels for selected health indicators. Most practices use evidence‑based national guidelines. Your Integration Specialist, working in consultation with physicians and specialists will define which targets to set for each indicator.
A gap in care exists when someone is overdue for a service that should be done periodically (known as a process care gap) or when a someone is not meeting the goal range for a particular disease or condition, such as having an blood level marker in a routine test higher or lower than the recommended target. Care gaps of selected indicators are identified from the gaps queries that your Integration Specialist will develop.
During preparation for health care appointments or during progress reviews with each person you serve, you will identify care gaps, discuss them with the person and update that individual's problem list to identify the unmet need and make plans to follow up.
Analyze Patterns, Trends and Outcomes
The Integration Specialist can use the Patient Registry to identify patterns and trends in specific areas of need. Some examples are:
- What interventions are having a positive effect on health and health management?
- What gaps currently exist in care management and resources for certain common conditions?
- How can we improve consistency and efficiency in supporting individuals to obtain needed health care for common conditions?
- What patterns exist for certain conditions for which more emphasis, staff training, and additional intervention might be
- warranted (for example, individual or group education services on diabetes prevention and management)?
- Are we using current internal and community resources effectively?
- What resources do we need to obtain or develop to improve supports where gaps exist?


What You Will Learn
Document Integrated Care Management services objectively and specifically in progress notes.
Use appropriate service types when documenting Integrated Care Management services.
General Guidelines
Integrated Care management documentation must describe Integrated Care management activities but objectives, specific and free of lingo. Specific and free of lingo means: describe specifically what you did, avoiding terms like "assessed," "referred," "linked," or "monitored" in favor of describing what you did, e.g. "read the custom time report and progress notes for ARMHS services," "scheduled an appointment with," "spoke with," etc.
For more information on writing high quality progress notes, see the section on documentation in this manual at Documentation and Electronic Health Records: Progress Notes.
Notes for Contacts
Use the following table for guidelines on what service types to use when documenting contacts with individuals for Iintegrated Management services. Only these services trigger billing for Case Mangement or Behavioral Health Home Services in a given month and at least one contact service must be provided each month.
When documenting services, you will be asked to select a meeting type. This determines the billing code. Face-to-Face or Telehealth Services are required at least once every 90 days for each person servec.
| Description of Activity |
Service Category |
Billable Service |
| Intervention and assistance provided previous to completion of the first Integrated or BHH Service Plan or other Interventions unrelated to current goals and objectives. |
Behavioral Health Home
Case Management |
BHH Intervention
CMGT Intervention |
| Regular ongoing services with an active plan |
Behavioral Health Home
Case Management |
Behavioral Health Home Services
Case Management |
| Assessment and Planning done face to face or by phone with the recipient |
Behavioral Health Home
Case Management |
BHH Assessment and Planning Interview
CMGT Assessment and Planning Interview |
Add-Ons to Contact Services
For any contact service provided face-to-face or by telephone, use these add-ons to identify service coordination or referrals made in conjunction with (during or immediately following) the service. When the add-on service occurs directly following a contact, include the time in the contact note and describe the add-on service in the intervention narrative.
Documenting Traveling From a Service Followed by an Add-on
If you provide an add-on service to services, but provide that add-on service after traveling back to the office, record your travel back to the office as Travel During Service. Explain this in your narrative. This is only allowed when the service, travel, and add-on service provided at the office are consecutive/contiguous (not uninterrupted by other activities). If you do something else in between, do not use an add-on, rather document the coordination, referral, or advocacy as a separate service at the precise time that it occured.
Standardized Add-Ons for BHH and CMGT
| Service Name | Use |
|---|
| Advocacy During or Following Service | When during or after a service you make advocacy calls, write emails, etc.
Overlaps allowed only with the service with which it is associated. (Meaning, you could provide this service in the middle of a split session where you speak with the client direclty before and after this activity while providing telehealth or phone services. Example: You have a direct (face-to-face or telehealh contact with the client. You then make some calls on the client's behalf, then you call them back or resume the service.) |
| Assessment & Planning Interview Write Up |
Use for time spent immediately following an interview to finish writing up findings, eliminating the need for another note. |
| Being Observed/Mentored During Service |
When Trainee is being observed while Trainee is providing a direct service. |
| Being Shadowed During Service | When Trainer is being observed, Trainer is providing the direct service. |
| Bus Pass Delivered |
Please remember this add-on whenever providing a bus pass to a client to avoid claims (as have been alleged in the past) that we are not delivering them to the clients for whom they are intended when they are delivered by mail to the office. |
| CMGT Pre Service Prep Work | May be used to account for time preparing for a service (reading assessments, gathering information, etc.) |
| Contact & Scheduling Related to CCN | Document efforts to contact a cllient who cancels or no-shows. |
| Coordination Related to Service |
When during or after a service you make calls, write emails, etc., to other service providers for purposes of coordination.
Overlaps allowed only with the service with which it is associated. (Meaning, you could provide this service in the middle of a split session where you speak with the client direclty before and after this activity while providing telehealth or phone services. Example: You have a direct (face-to-face or telehealh contact with the client. You then make some calls on the client's behalf, then you call them back or resume the service.) |
| COVID Vaccine Assistance Offered | Very important to document our efforts to assure that clients get the help they need. |
| Dental Care Appt During Services | When attending an appointment with client. |
| Incident Report Filed | Very important to document when incidents are reported. |
| Insurance Advocacy During/After Service | When during or after a service you provide assistance maintining or restoring health insurance coverage.
Overlaps allowed only with the service with which it is associated. (Meaning, you could provide this service in the middle of a split session where you speak with the client direclty before and after this activity while providing telehealth or phone services. Example: You have a direct (face-to-face or telehealh contact with the client. You then make some calls on the client's behalf, then you call them back or resume the service.) |
| Primary Care Appt During Services | When attending an appointment with client.
|
| Progress Review in Session | Progress review should always be done with clients. Use this add-on to demonstrate that. |
| Recovery Team Meeting |
Client must be present. |
| Referral During or Following Service | When during or after a service you make referrals to services at Accend or to other providers.
Overlaps allowed only with the service with which it is associated. (Meaning, you could provide this service in the middle of a split session where you speak with the client direclty before and after this activity while providing telehealth or phone services. Example: You have a direct (face-to-face or telehealh contact with the client. You then make some calls on the client's behalf, then you call them back or resume the service.) |
| Specialist Care Appt During Services | When attending an appointment with client. |
| Travel |
Use only for direct services provided at a location other than one of our offices. |
Non-Contact Activities
Use the following service types for activities that do not include contact with individuals. These activities other than the last, while vital to the services, do not trigger a billing record for the service for the month.
| Note Type |
Use For |
| Referral Intake Discharge |
Conducting an intake interview prior to a DA or established eligibility for case management, or activities related to discharge, writing a letter to the individual who has disengaged and lost contact, clerking the client status or other information in the EHR, etc.) |
| Eligibility Screening |
All activities associated with conducting and eligibility screening, including obtaining ROIs, gathering information, and writing the screening document. |
| Contact and Scheduling |
Telephone or written efforts to contact referrals or individuals currently served. |
| Case Management Assmt No Contact |
Writing the Functional Assessment, ICSP (Integrated Sevice Plan) or Progress review while not with the individual served. Reviewing previous assessments or plans while preparing for an interview or update. |
| Referral to Services |
Any conversations with the individual served about recommended services, or formal referrals to service providers. This may overlap with other activities. When this occurs during a direct service, use the Add-On referral type described below. |
| Service Coordination |
Monitoring and coordinating health care, mental health, residential, vocational, or other services, or talking with providers. When this occurs during a direct service, use the Add-On referral type described below. |
| Advocacy No Contact |
Advocating on behalf of individuals served with law enforcement, landlords, county financial workers, and a variety of other community members who are not direct service providers. |
| Insurance Advocacy |
Advocating on behalf of individuals served specifically regarding health insurance coverage. |
| Cancellation By Provider |
Cancellation of a planned appointment by you for any reason. |
| Client Initiated Cancellation |
Cancellation of a planned appointment initiated by the individual |
| File Note |
Miscellaneous recording of necessary information about an individual not fitting another category. |
Case Management Mentoring
Case Manager Associates must receive 5 hours of mentoring per week from a qualified Case Manager (includes Mental Health Professional who qualifies as a Case Manager). Mentoring may (and should) occur during Case Management service provision (the service is allowed to overlap with others.
The mentor should document Case Mgt Mentoring Others, and indicate on the note who is being mentored. The Associate should document Case Mgt Being Mentored, and indicate on the note who is doing the mentoring. These note types take place during other Case Management Activities.
| Service Type |
Detail |
| Case Mgt Mentoring Being Mentored |
A Case Management Associate performing work in the presence of, or consulting with, a Case Management Mentor. |
| Case Mgt Mentoring Others
| A qualified Case Management Mentor consulting with or observing a Case Management Associate. |

What You Will Learn
Conduct global progress review and quality assurance that examines the outcomes of all health care, mental health, residential and vocational or educational and other services a recipient of Integrated Care Management recieves.

Integrated Care Management progress review and quality assurance is not limited to simple twice-per-year updates of required assessments and the ICSP.
Rather, it is an ongoing process that should be characterized by review of all of the health care, mental health, residential and vocational or educational and other services a recipient of Integrated Care Management needs, and is receiving.
Integrated Care Plan Review and Update
A well-crafted Integrated Care Plan has identified the individual's current strengths and resources, and needs for services. Good Integrated Care Management is seeing to it that the individual is referred to, engaged in and receiving high quality services. The Integrated Care Plan review is a review of all of those services. As follows:
- Referrals: have you, with the individual's permission, made referrals for the services recommended in the DA, FA and ICSP?
- Responsiveness: have the providers to whom you have referred, done their part to deliver the services they have been asked/they have promised to provide?
- Engagement: is the individual satisfied with, engaged and participating in the services to which he or she has been referred?
- Progress: is the individual making progress on the goals and objectives for this service that are listed in the ISCP as well as in the Treatment plan for that specific service?
- Changes needed or additional services: depending on the answers to all of the above, what changes or additional services are needed?
The Integrated Care Manager's Role in Coordinating the Recovery Support Team
Especially when an individual receives more than one service from Accend, but also in cases where he or she receives these services from other providers, Integrated Care Managers should schedule Recovery/Support team meetings to review progress toward recovery and treatment goals. The most appropriate times to hold such a meeting are
- at the time of the Interview for a DA Update;
- when a recipient experiences a significant life change, such as moving to a higher or lower level of care;
- when treatment progress is significant and/or discharge from case management or other services may be recommended;
- when treatment progress is slow or stalled and may require changes in services or methods;
- other significant changes or events in the lives of Case Management recipients.
-
Recording Support Team Contacts
TabsTM provides a utility for recording all of the key contact persons for persons served. Integrated Care Managers should keep this contact list up-to-date with all external service providers, family members, and other natural and formal support persons in each individual's support network and whom we may need to contact on behalf of recipients. Find this utility in the Client Info section.

What You Will Learn
Provide active and responsive services during transitions and placements
Assure continuity of care during transitions
As Integrated Care Manager, you are the lead facilitator and coordinator of the individual's support and treatment network during periods of transition and placement. We expect you to take an active role in facilitating successful transitions and placements with the goal of assuring successful transitions, and the best possible treatment outcomes in placement, and successful discharge planning.
Moving
When you learn of person's desire to move to a new area, your job is to immediately begin assessing the individual's needs (for housing, supports, services, etc.) in the new location and helping the individual to begin locating these resources prior to the move. This assessment and planning should include:
- Housing in the new location
- Financial supports and services and basic needs
- Arrangements for health insurance if a change in providers will be necessary
- Referrals to Case Management Services
- Referrals to other medically-necessary mental health services
- Referrals to health care services
- Arrangements for transportation
- Other
Continuity of Services
Following the move, if the individual remains in Minnesota, we follow-up with and continue Integrated Care Management services in the new location until the individual has obtained services with the new provider.
If the individual receiving services moves to a location where we provide te same services, offer and make arrangements for a transfer to an Accend Case Manager in the new location if that is what the person wants.
If the individual is moving to an area where we cannont provide Case Management services based on the individual's insurance or because we do not have a presence in the new location, offer one of two options:
- Offer BHH Services in the new location if we have a BHH presence there.
- Contact the new county of residence about Case Management resources and make referrals according to that county's process. Continue services in the new location (for not longer than 60 days, or until a new provider has been located and services have begun, coordinating with the new provider to make the transition, handing over the case on the first of the month.
Travel to the new location to provide services is allowed. Communicate with your supervisor about the frequency of necessary travel. Help the individual locate and use resources for the move. Provide services by telephone where possible, traveling to the new location only as necessary.
If the individual is moving to another state, do research on options for mental health services available in that state, and help the individual connect with these services prior to the move.
Temporary Residences in New Locations
Some moves are temporary. These include moves to residential treatment, foster care, board and lodge, and other types of placements because placements in these facilities do not establish residency in the new county. When a move is temporary, continue Integrated Care Management services in the new location, unless the individual requests, and the payer (the host county or Managed Care Organization) agrees to a transfer the case.
Hospitalization
When an individual is hospitalized, the Integrated Care Manager's role includes:
- Supporting the individual in communicating needs with hospital staff
- Communicating and coordinating with hospital social workers on successful treatment and discharge planning
- Making arrangements for housing, supports, follow-up care, transportation and other necessary services post-discharge
- Obtaining, with the individual's permission, discharge instructions, and supporting him or her in obtaining resources to follow them.
Placement in Residential Treatment
Your role as a Integrated Care Manager when an individual enters residential treatment is to be the central coordinator of treatment and care in the facility, treatment and discharge planning. Do all of the following:
- Obtain ROIs for communication with the treating facility prior to, or immediately upon admission.
- Provide assessment (Diagnostic, Functional, etc.) to the facility for use in treatment planning.
- Help the individual locate resources for care of his or her home, pets, family members, or other needs as necessary during the placement.
- Arrange for transportation to the facility.
- Arrange to attend initial treatment planning meetings at the facility, and make a plan for frequency of contact with the individual during the placement.
- Make regular contact with the individual and facility staff to monitor progress.
- Attend progress review and discharge planning meetings.
- Make arrangements for transportation upon discharge, and post-discharge housing, aftercare and other supports as needed.
Placement in a Nursing Facility
When a recipient of Integrated Care Management services is placed in a nursing home temporarily (with an anticipated placement of less than 180 days) continue Integrated Care Management services, with responsibilities matching those of hospitalization, above. When the individual is placed long-term, arrange for a transfer of services to the nursing facility staff and social workers.

What You Will Learn
Use required steps to discharge a recipient when the individual
has achieved goals and objectives and stability in status and functioning;
has moved or disengaged from services; or
is no longer eligible for other reasons.

Disharge from Integrated Care Management may occur in any of the following circumstances:
Administrative Discharge
Administrative Discharge occurs when a recipient ends services for any of the reasons listed below. In these cases, discharge immediately or as indicated in the specific line items (no 6-month closing period as for disengagement).
- Voluntarily chooses to discharge.
- Becomes irreparably and permanently uninsured for AMH-TCM services, and connected to service and support resources elsewhere
- Moves out of state
- Moves or has been out of contact for a period of one month or more and contact is not possible because the client does not have a phone and we have no known address, or any collateral contact persons associated with the individual. In this case leave the case open (in Closing status) for 6 months from last contact, as for disengagement.
- Moved to another county in the state where we do not have an Integrated Care Management presence. Before discharging for such a move, complete all of the following steps:
- Assure the recipient that we will continue to provide services to him or her in the new residence for at least 60 days, or until he or she is connected with services in the new location.
- Do not discharge a recipient who moves to an excluded time facility. These include:
- Hospitals
- Sanitariums
- Nursing homes
- Halfway houses
- Foster homes
- Board and care homes
- Maternity homes
- Domestic violence shelters
- Regional treatment centers
- Do not discharge the recipient if the move is temporary (less than 60 days) and the recipient will return within 60 days to his or her original county.
- Chooses a service that is incompatible with AMH-TCM or BHH services (such as Assertive Community Treatment).
- Is arrested, convicted and incarcerated.
- Has been civilly committed and is receiving case management services from the county.
- Has transferred to Case Management or BHH services to another provider.
- Has requested discharge for another, documented reason.
Is no longer eligible for services for other administrative reasons.
Clinical Discharge

Consider BHH Services
When discharging based on a finding in a recent DA or Eligibility Screening that Case Management Services are no longer medically necessary:
Consider that the individual may still be eligible for and need Behavioral Health Home Services.
If so, offer BHH services and transfer the case if the individual accepts. If the current Case Manager is competent to provide BHH services, no change of primary is needed. Complete the CMGT discharge and get to work immediately on BHH assessments.
Clinical Discharge occurs when the recipient:
- Has achieved his or her goals/outcomes and reaches a level of psychiatric stability and status so that Integrated Care Management services are no longer necessary, and has participated in a voluntary successful discharge process, including connections to formal and informal ongoing supports
- No longer qualifies based on a Diagnostic Assessment and Eligibility Screening using the eligibility requirements above during an recently-updated Diagnostic assessment that determines services are no longer necessary, and has been informed of the finding, and received information about appeal rights.
- *Do not discharge a client from Targeted Case management sevices for clinical reasons until two subsequent updates to the Diagnostic Assessment indicate the individual no longer needs this level of care. The eligibilty screenining for TCM lasts three years. This makes sense. It allows for maintenance and stability before discharge or a change to a different level of care.
- Has repeatedly declined to participate in assessment updates to maintain ongoing eligibility determination, with documented evidence of effort to schedule and conduct the session, including offering to provide the assessment at home as needed, arranging transportation, etc.
- Has needs that will be met better by another agency, and has been referred and admitted for services with that provider.
- Voluntarily chooses to discharge. In this case, another party (Treatment Supervisor, another service provider, Case Management Lead, or Service Coordinator might best contact the person to obtain more information about why the individual is choosing to discharge at this time.
- Has disengaged from services for a period of six months or more, with documented efforts to contact, schedule, re-engage and coordinate with other service providers within and outside the agency. In this case, take the following steps prior to discharge:
- Someone other than the assigned Integrated Care manager attempts to contact the individual investigate the reasons for disengagement.
- Make efforts to re-engage the recipient through other service providers or the referral source.
- If contact is lost, send a letter to the recipient's last known address, offering services and inviting the recipient to re-engage at any time.
- Move the recipient to Closing status if disengaged for a period of two months.
- After a period of 6 months send the recipient a second letter informing him or her of discharge and inviting him or her to contact us at any time in the future.
- Complete a Discharge Progress Review and changethe individual's status to Previous.
Planned Discharge
For planned discharges, complete a Discharge Progress Review.
Appeals, Grievances and Complaints

What You Will Learn
Inform an individual about his or her appeal rights when found ineligible for Case Management or BHH services.
Handle a recipient complaint or grievance about Integrated Care Management services.
Assist a recipient in filing a grievance with Minnesota Medical Assistance or a Managed Care Organization.
Eligibility Screening Appeals
Any referral to or current recipient of Case Management services who is found ineligible for Case Management services as a result of a Diagnostic Assessment or screening may appeal this decision.
Complaints or Greivances
Any recipient of Case Management services may file a complaint or grievance about his or her Case Management, other mental health or health care services, or about actions or decisions taken by his or her payer (Medical Assistance or a Managed Care Organization) at any time.
Integrated Care Managers should assist any client who wishes to file a complaint or grievance. He or she may do so with an internal grievance that will be reviewed by an administrator at Accend, or she or she may file a compliant or grievance with her or her payer, using the resources below.
Payer Resources for Grievances or Complaints
Supervision of Integrated Care Management Services must adhere to the requirements for the service being billed. Current policy is that each client's services and progress are reviewed every 60 days from the previous plan.
When the service being billed is Targeted Mental Health Case Management, supervision must be conducted by a Licensed Mental Health Professional. An RN may be asked to consult on certain cases.
When the service being billed is Behavioral Health Home Sevices, supervision must be conducted by the Integration Specialist (Registered Nurse). An MHP may be asked to consult on certain cases.
When an individual receives Behavioral Health Home Services and a Mental Health Service (ARMHS, CTSS, EIDBI, or Psychotherapy) the supervision should be conducted jointly.
Review and Approval of Assessments and Plans
Depending on the service being billed, the following approvals/signatures on Assesssments Service Plans are required:
- For AMH-TCM clients, only Licensed Mental Health Professional's signature is required on the Functional Assesssment and Treatment Plan.
- For BHH-only clients, only the (RN) Integration Specialist’s signature is required on the HWA and Service Plan. The RN may request consultation on these clients from the MH Professional, just as the MHP may request consultation from the RN on ARMHS, CTSS, CMGT and other services.
- For Integrated Plans that include BHH and clinical mental health treatment services, signatures of both the RN and MHP are required on the FA/HWA and Plan. In these cases, the MHP and RN can collaborate by reviewing and approving appropriate sections of the assessment, or objectives, then changing the assigned reviewer to their corresponding partner. Once both have reviewed, the final reviewer may approve the assessment or plan. Preferred is that the MHP approve/sign these plans electroniically and the RN signs the completed document using our signature tool.
Case Management Qualifications
Case Manager
Case Managers at Accend must have bachelor's degree in one of the behavioral sciences or related fields including, but not limited to, social work, psychology, or nursing and have at least 2,000 hours of supervised experience in the delivery of services to adults with mental illness.
A case manager must receive regular ongoing supervision and treatment supervision totaling 38 hours per year of which at least one hour per month must be treatment supervision regarding individual service delivery. The remaining 26 hours of supervision may be provided by a case manager with two years of experience.
Case Manager Trainee
A Case Manager Trainee is a Case Manager with a degree without 2,000 hours of supervised experience in the delivery of services to adults with mental illness. A trainee is not an associate, but must:
-
receive treatment supervision regarding individual service delivery from a mental health professional at least one hour per week until the requirement of 2,000 hours of experience is met; and
-
complete 40 hours of training approved by the commissioner in case management skills and the characteristics and needs of adults with serious and persistent mental illness.
Case Manager Associate
There are various qualifying criteria defined for non-degreed Case Manager associates defined in Minnesota Statute 245.462. These include the following mentoring and continuing education, supervision, and mentoring requirements:
- 40 hours of preservice training described under paragraph (e), clause (2);
- at least 40 hours of continuing education in mental illness and mental health services annually; and
- at least five hours of mentoring per week from a case management mentor*, and
- receive treatment supervision at least once a week
*A "case management mentor" means a qualified, practicing case manager or case management supervisor who teaches or advises and provides intensive training and treatment supervision to one or more case manager associates. Mentoring may occur while providing direct services to consumers in the office or in the field and may be provided to individuals or groups of case manager associates. At least two mentoring hours per week must be individual and face-to-face.
Behavioral Health Home Staff Qualifications
Registered Nurse with 4 year BA or BS degree. The Integration Specialists meets regularly with the Integrated Care Managers, meets all Behavioral Health Home recipients, reviews the Health and Wellness Assessment and co-approves the Integrated Care Plan and subsequent updates along with the mental health Treatment Supervisor.
A case manager as defined in Minnesota Statutes, section 245.4871, subdivision 4 (excluding paragraph a), and Minnesota Statutes, section 245.462, subdivision 4 (excluding paragraph a), or
A mental health practitioner as defined in Minnesota Statutes, section 245.4871, subdivision 26 or Minnesota Statutes, section 245.462, subdivision 17
The Behavioral Health Home specialists partners with a Behavioral Health Home Specialist to provide the supports identified in the Health Action Plan, reporting progress and results, and identifying new needs or concerns to the team.
Health Home Specialists will assist Navigators in implementing the supports identified in the Health Action plan, including helping individuals prepare for and attend appointments, teaching self-advocacy skils and Heath and Wellness education. Advocating on behalf of individuals as needed to obtain necessary medical care.
Qualifications for the role include:
A community health worker as defined in Minnesota Statutes, section 256B.0625, subdivision 49
A peer support specialist as defined in Minnesota Statutes, section 256B.0615
A family peer support specialist as defined in Minnesota Statutes, section 256B.0616
A case management associate as defined in Minnesota Statutes, section 245.462, subdivision 4,
paragraph (g) or Minnesota Statutes, section 245.4871, subdivision 4, paragraph (j) (unless the individual is a Mental Health Practitioner and therefore qualifies as a Systems Navigator)
A mental health rehabilitation worker as defined in Minnesota Statutes, section 256B.0623,
subdivision 5, clause (4)
A community paramedic as defined in Minnesota Statutes, section 144E.28, subdivision 9, or
A certified health education specialist
Overview
The Behavioral Health Home Service Coodinator provides a central point and contact and communication for individuals served, provider staff, and community parnters, maintains medical records, promotes and coordinates rapid response to referrals, and reports on quality assurance priorities identified by the team and agency.
Responsibilities
Conduct intake interviews and brief needs assessments with referrals when Systems Navigators are not available.
Monitor referrals from referral to engagement, and all necessary assessment and planning. Report weekly to the Integration Specialist, Program, and Executive Director on referrals and engagement.
Receive and maintain medical records, transcribing applicable elements to the TabsTM EHR, and notify provider staff when key records are received.
Develop an articulate health and wellness vocabulary that will engender confidence in providers of health care and social services to the individuals we serve in common. Nurture positive and productive partnerships with providers with proactive communication and by providing information and education about the Behavioral Health Home Service, its purpose, goals and benefits to persons served.
Receive, route calls, and forward information from individuals served when they are unable to reach provider staff.
Facilitate coordination with the consumers’ Minnesota Health Care Programs (MHCP) managed care plan, if applicable.
Provide quality assurance reports at intervals identified on quality assurance goals and objectives for the Behavioral Health Home Service.
Maintain certification as a MNSure Navigator and assists individuals with maintaining health insurance.
Qualifications
The Service Coordinator will have at a minimum, the qualifications of a Qualified Health Home Specialist. Experience or training as a Health Unit Coordinator is a plus.
Resources
This guide is a living document. We want to improve it with your help. Do you have questions? Found a typo? Find yourself wanting more information? Please send us your thoughts about anything in this chapter by tapping on the link below.
Updates to this Guide
May 19, 2022:
1) Add-ons standardized and explained in more detail.
2) Scheduled Service No Show with Travel added to non-contact service list as a billable service for Case Management.
November 28, 2022:
Eliminated reference to the Service Intensity Assessment in required assessments.
January 19, 2023:
Language corrected in required assessments for BHH: annual DA not required.
February 14, 2023:
Supervision of ICM Services clarified.
March 28, 2023:
Process for Initiating BHH services clarified to require Authorization forms prior to eligibility review.
May 1, 2023:
Language clarification in eligibility table. No change of rules.
January 25, 2024:
Correction to requirement for updates to the Diagnostic Assessment for Case Management. A update to the DA is required only every three years.
June 11, 2024:
Broken links to external resources for Immunizations and Preventative Health Care fixed.
Links to other obsolete guide sections removed.
Clinical Supervisor/Supervision replaced with Treatment Supervisor/Supervision to align with uses of this phrase in other services
August 22, 2024:
Functional and Health and Wellness deadlines for updates clarified based on July 1, 2024 statutory changes (updates required every 365 days after the full Functional or Health and Wellness assessment, where previously this was every 6 months).
September 19, 2024:
BHH and CMGT Intervention While Initiating notes changed to simply Intervention. Instructions clarified as applicable for other interventions.
January 8, 2025:
Intake process clarified to obtain client consent on Rights and Responsibilities form during intake interview.
January 16, 2025:
Contact With Identified Supports described as a billable contact for BHH services, and requirements described.
February 28, 2025:
Requirement for Diagnostic Assessment prior to admission corrected to with the past 12 months, where it previously said 6 months.