Adult Rehabilitative Mental Health Services

The focus of Adult Rehabilitative Mental Health Service is recovery. ARMHS teaches skills to develop and enhance psychiatric stability, social competencies, personal and emotional adjustment, and independent living and community skills, when these abilities are impaired by the symptoms of mental illness.
While improved functioning is the primary goal of ARMHS, for some of the people we serve, significant impairments in functioning may continue chronically. For these individuals, the focus of ARMHS may be to help them make changes in their environment, use formal and informal supports more effectively, improve health and health care, and more effectively use mental health, health care, social services, and other supports to accommodate deficits in functioning.
When recipients of ARMHS receive other mental services, Psychotherapy or Case Management, for example, ARMHS supports these services with the skill development needed to achieve the goals and objectives identified in their Psychotherapy Treatment Plans or Case Management service plans.
Read more about ARMHS now in the Minnesota Health Care Programs Manual, ARMHS Chapter, here.
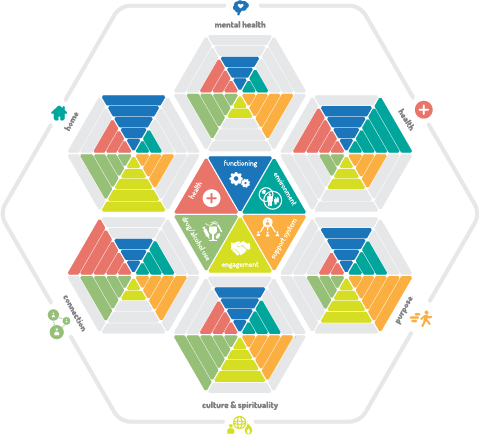
Persons eligible for ARMHS are diagnosed with Serious or Serious Persistent Mental Illness that impairs functioning in at least two domains of independent living. These domains are defined by statute and include those listed below. (At Accend, we include other domains in our assessment and treatment planning process.)
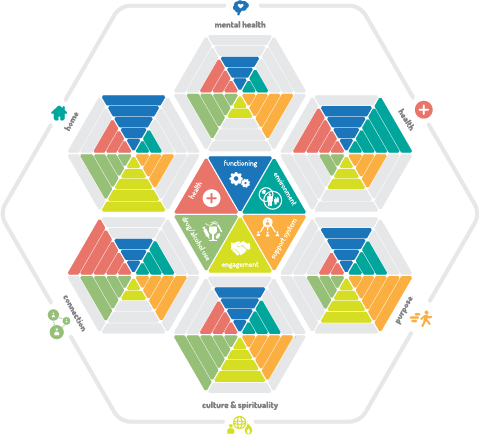
- Mental Health
- Symptom Management
- Accessing and Using Mental Health Services
- Health
- Health and Dental Care
- Avoiding Abuse of Drugs and Alcohol
- Home
- Obtaining and Maintaining Housing
- Money Management and Accessing Financial Assistance Resources
- Transportation and Transportation Resources
- Self-Care Independent Living Skills
- Connection
- > Interpersonal Functioning and Communication, including:
- - Friendships and Relationships
- - Family Relationships and Parenting, and
- - Self-Advocacy
- > Healthy Social and Leisure Skills
- Purpose
- > Work and Vocational Readiness Skills, or
- - Volunteering and Civic Involvement
- > Education
- Culture and Spirituality
- > An extension for some, of Connection and Purpose, and/or
- > A key element in recovery

What You Will Learn
Meet deadlines for ARMHS assessment and planning
Conduct a functional assessment that
Assessment and treatment planning for ARMHS is not a compliance exercise. Rather, high-quality assessment, and a person-centered treatment plan that is strengths-based, goal-oriented, and recovery-focused, improves the quality of services and assures that ARMHS are measurably rehabilitative.
ARMHS begin with a Diagnostic Assessment that establishes initial eligibility and recommends ARMHS as medically necessary. The Functional Assessment begins immediately following the DA and referral. The FA confirms eligibility by identifying an individual's current strengths and resources, immediate needs, and the domains in which functioning is impaired by symptoms of mental illness, forming the basis for effective treatment planning.
Treatment planning in ARMHS begins with helping individuals identify long-term goals and a recovery vision. While we have defined recovery in broad terms above, keep in mind that recovery is defined individually for each person we serve, and by his or her goals.
Read about person-centered assessment now, in the Assessment and Planning section of this guide, here.
Assessment and Planning Deadlines for ARMHS
ARMHS requires the following assessment and planning deadlines. We encourage you to complete assessment and planning ahead of deadlines when ever possible.
| Item |
Initiating Services (New Referrals) |
Update |
| Diagnostic Assessment |
Upon Admission
*ARMHS services may begin immediately after the interview, but the DA must be completed (approved) within 5 days of the 2nd ARMHS appointment.
A recent DA may be used for admission. For our purposes, a recent DA is one that has been completed in the past year, and where the referred has not encountered significant life changes, mental-health related hospitalizations or residential treatment, crisis placements, commitments, or other significant changes in mental health status or symptoms since the last DA.
Use the Intake DA for referrals new to Accend.
|
Reviewed annually and a new DA conducted if recommended by the conclusions of the reviewer. |
| Functional and Health and Wellness Assessment |
Within 30 Days of Admission
Use the Intake FA/HWA for referrals new to Accend.
If the person you serve also receives Case Management or Behavioral Health Home Services, the Case Manager/Systems Navigator will complete this assessment, or ask you to collaborate on it.
|
Every 365 days, or
if the individual exhibits significant changes in functioning, or experiences a significant life change (such as moving, serious health condition, etc.) meriting an update to the FA/HWA. |
| Client Status Assessment |
Within 30 Days of Admission
Once embedded in the FA, this is now a stand-alone assessment only.
|
Every 180 days |
| Level of Care Assessment |
Diagnosticians: see guidance in the MHCP manual here.
|
Each Diagnostic Assessment |
| ARMHS Treatment Plan |
Within 30 days of admission
If the referral has a Case Manager who is completing the FA, you may begin immediately with Treatment Planning.
After work on the FA is done, document your next visits with a new referral as Treatment Planning Initial Interview. This may still include getting started with connecting him or her with resources to meet basic needs (housing, food, health care, etc.)
If the person you serve also receives other services, coordinate other providers to develop an Integrated Plan.
|
Every 180 days
Complete a Progress Review every 60 days. |
Definition of Active Treatment
ARMHS is an Active Treatment service. Active treatment in ARMHS includes activities that are directed toward:
- Identifying symptoms and developing coping skills
- More effectively using health and mental health care services
- Meeting immediate unmet basic needs with an emphasis on preventing future unmet needs
- Developing increased skills, healthy habits and routines, and increased independence in the domains listed in the Functional Assessment
- Maintaining current optimal functioning to the maximum extent possible and preventing relapse, or loss of current functional status or independence
- Reducing risk of hospitalization, use of crisis response resources or placements, or long-term residential treatment
- Improving status and increased independence in housing, employment, and/or education

A Note on Traveling (Ridesharing) With ARMHS Recipients
You may find that while providing ARMHS, recipients ask for rides. At times, individuals have come to expect rides because they have received them in the past.
Transportation is not an ARMHS service. Rather, helping individuals identify and connect with resources for transportation (public transportation, med cabs, or other) and teaching them how to access and use them should be a part of the Treatment Plan when needed.
But because individuals ask or expect rides, you are placed in the uncomfortable position of having to say "no," or giving the ride to avoid conflict. Avoid this proactively by defining up front, in the ARMHS Treatment Plan, where and when you might rideshare. By making it clear where you might travel with the people you serve, proactively, when developing the Treatment Plan with them, you might find that this will make it easier to avoid these uncomfortable requests, or at least help you, if you are asked, to be more confident in answering.
Ridesharing with a client in your car is allowed. Ridesharing means travel during services to a location you are traveling and sharing a ride there is the more efficient option than traveling separately. Ridesharing is allowed only with these requirements and restrictions:
- The location to which you travel must be a place where you provide an ARMHS service,
- that is described in the Treatment Plan,
- including the location specifically, or sufficiently enough described in the methods in the plan,
- to demonstrate the medical necessity for services in that location, and
- be a location that the individual you are serving would otherwise (naturally) access, if not ridesharing with you.
When ridesharing during an ARMHS service, document your mileage as travel during in the Progress Note.
Active treatment is not occurring when individuals:
- Are not involved in activities that address their individualized priority needs
- Do not have opportunities to practice new or existing skills and make choices in their daily routines
- Are not demonstrating progress toward the goals and outcomes in the Treatment Plan and/or progress in at least one of the 6 ratings in at least one domain the 6X6 Functional Assessment
- Are not developing new skills and healthy habits in spite of interventions, and after thoughtful review and modification of the Treatment Plan in response to the lack of progress
Temporary setbacks and relapses might be expected with some individuals. When these setbacks occur, they do not negate previous success. Rather these are opportunities to step back, reset, learn about triggers for relapse, and revisit and improve the Relapse Prevention or Crisis Response plan.
Responsiveness to Immediate Needs
ARMHS begin with a Diagnostic Assessment that identifies a mental health diagnosis, and makes initial treatment recommendations. At Accend, each new referral receives an Intake Interview along with the DA. The Intake Interview identifies the reason the individual has come to us for services, and assesses immediate, unmet basic needs.
Begin ARMHS by responding to those unmet basic needs. Conduct initial assessment and treatment planning while helping the individual to connect with resources, services and supports to meet these needs.
Adherence to the Treatment Plan
The ARMHS Treatment Plan is a description of medically-necessary services. Think of it as a prescription. Would a doctor prescribe medications and instruct the patient to take only some of them? Your Treatment Plan describes services, frequency, duration and methods. Your services to any individual should closely match that plan.
If they don't, your responsibility during Progress Review is to examine why not, and, if necessary modify the plan. Examine:
- Are services exceeding the planned frequency and duration because many crises and needs are requiring more services than were planned? What other services or resources might he or she need to prevent this?
- Is the person not participating in as many services as planned, perhaps canceling frequently, and if so, why?
- Is he or she busy, employed, or otherwise unable to participate?
- Have you been person-centered in planning dates, times and locations that work for him or her?
- Does the plan recommend more services than the individual really desires or has the motivation in which to participate at this time?
- Are your services meeting his or her needs? Is the plan person-centered?
- Are you scheduling appointments that match the frequency and duration recommended in the plan? Have you set a regular, repeating appointment with him or her to help make services more consistent?
- Other factors and considerations. Your services should match the Treatment Plan.
When service frequency and duration does not match the Treatment Plan, please seek guidance from your supervisors on how to respond to and correct this deficiency.
ARMHS Special Services

Community Intervention
Community Intervention is interventions with others (3rd parties) on behalf of the individual to whom you provide ARMHS. You might learn from an individual you serve that he or she is:
- at risk of hospitalization or placement in residential treatment that may be avoidable with intervention;
- at risk of losing housing;
- at risk of losing a job;
- at risk of losing essential services for survival, health, and safety; or
- facing other imminent events that threaten independent living status.
You take action to eliminate or reduce these risks, advocating, and solving problems on behalf of the person you serve. This is Community Intervention.
This is the only ARMHS service that you may provide that may not include direct (face-to-face) contact with the recipient. In these cases, you intervene with a relative, guardians, friend, employer, landlord, treatment provider or other significant people to change situation. You might provide these interventions face-to-face or by phone with these individuals and this may occur with or without the individual present.
Do not use Community Intervention if you do not intervene with others. Keep interventions to 40 minutes or less.
Community and ARMHS Individual on the Same Day
Community Intervention can take place on the same day as another service. Let's say that you meet with someone who is experiencing a problem and needs intervention. You work with them to practice skills for managing the stress or anxiety stemming from the crisis: ARMHS Symptom Management. Later, you intervene with or meet with that provider to address the problem: Community Intervention. As long as the services do not overlap, they may be billable separately.
Cases like this are not always separately billable. You may make calls with the individual experiencing the problem, coaching on communication or self-advocacy, or anxiety management skills. This is also ARMHS, if such skills are part of the treatment plan, but is not a separate Community Intervention, because the work was with, not on behalf of, the individual.
Billing Community Intervention
We bill Community intervention to the payer as an occurrence per day, at the equivalent of 45 minutes, and most interventions should be take less time than this. Seek permission from your supervisor for interventions that will take longer than 45 minutes.
Do not use Community Intervention for routine service coordination activities, Treatment Supervision or consultation. If you have questions about whether or not an intervention you provide constitutes a Community Intervention, ask your supervisor.
New Referrals with Immediate Unmet Basic Needs
When you begin work with someone who has immediate unmet basic needs, you will respond by connecting them to supports and resources. This includes supports for connecting them with help obtaining insurance. This help is not community intervention unless it conforms to the definition above.
Helping individuals with unmet basic needs, identifying what resources and supports they currently have and what are the barriers to them getting needs met is part of functional assessment. While you provide these supports, record what you learn in the Functional Assessment, and document your time as Functional Assessment Interview.
Seek Guidance
If after reading this guide, you still have have a question about when to bill Community Intervention as a unique service, seek advice from your supervisor.
Transition to Community Living
Transition to Community Living requires prior-authorization. Before providing services to someone in a hospital or facility, talk to your supervisor.
Transition to Community Living is the only ARMHS service you may provide to a recipient who is in a hospital, residential treatment (IRT) facility or other MA-funded medical facilities including the following:
- Regional Treatment Center
- Community hospital
- IMD
- Intensive residential treatment program
- Board and care facility
- Skilled nursing home
- ACT program
It is not a routine ARMHS service, rather it is a service that is intended to support the individual's successful discharge from the facility. Transition to Community Living services might include, but are not limited to the following, so long as these services do not duplicate treatment services provided by the facility.
- Establishing or maintaining contact with the person who is placed in the facility
- Helping the individual who is placed communicate with the provider and advocate for needs
- Helping the individul identify and use strategies that will improve success of the placement and shorten the duration of the placement
- Discharge and aftercare planning
When to Use Transition to Community Living Services
Use Transition to Community Living Services when an current active client moves temporarily to an MA facility (for a stay of fewer than 180 days), or an individual in a facility is referred for ARMHS as discharge is drawing near, and ARMHS TCL services are needed to assist in planning/facilitating successful discharge.
When an ARMHS referral or recipient also has Case Management or Behavioral Health home services, these services may serve instead of ARMHS TCL for planning/facilitating discharge.
Transition to Community Living Services require a Treatment Plan identifying the need, goals and objectives for the services, methods and strategies, and frequency and duration of the services.
Transition to Community Living - Community Intervention
When an Individual is placed in a facility, brief inteventions on the individual's behalf, with employers, landlords, and others that meet the definition of Community Intervention above are also allowed. This service may also include advocating on behalf of the individual with factility staff to ensure success of the placment and expedite discharge.
Service Coordination
Coordination ARMHS with other health care, mental health care, social services, residential, vocational and educational supports is essential to successful treatment outcomes. Below are just a few of the ways that well-coordinated ARMHS can improve the outcomes of other services and supports.
Psychotherapy
When a recipient of ARMHS also receives psychotherapy, the ARMHS plan should directly support psychotherapy goals. Where an individual might be learning about symptoms and developing goals and strategies for coping with his or her psychotherapist, ARMHS can provide coaching and skill development between psychotherapy sessions for those strategies, Or, where other impairments in functioning are barriers to psychotherapy recovery goals, ARMHS can provide supports to reduce or eliminate these barriers.
Case Management
The ARMHS Treatment Plan should closely align with the Case Management ICSP, or Individual Community Support Plan. Where the ICSP identifies broad goals and accomplishments, and connects individuals with services and supports they need to achieve stability, optimize functioning and improve health and quality of life. ARMHS provides the skills training where impaired functioning is a barrier to these same goals.
Health Care
Where an individual's physical health impacts mental health, or is impacted by mental health symptoms, ARMHS can improve overall health outcomes if closely coordinated with health care services.
Residential Care/Housing
Many ARMHS recipients may live in supported housing, while others may be tenuously housed and at risk of losing housing. At Accend, we have a history of working cooperatively with housing providers to help individuals succeed in current housing, and achieve more independence and stability in housing.
Educational and Vocational Services
When a recipient of ARMHS is working, seeking work, or attending school, ARMHS can identify and work with recipients on removing barriers to work or educational readiness and performance. ARMHS is not job-coaching, and educational institutions most often have onsite supports as well, but when ARMHS is well-coordinated with these services, it can improve an individuals readiness and ability to use these supports effectively.

Use the following service types to document ARMHS:
| Service Name |
Use For/When |
Billable/ Target Time |
| ARMHS Cancellation By Provider |
You cancel an planned/scheduled appointment with a recipient. |
No |
| ARMHS Client Intiated Cancellation |
Your client cancels the appointment or is a no-show. |
No |
| ARMHS Community Intervention |
When you provide Community Intervention as defined in this guide. |
Yes |
| ARMHS Community Intervention by Wkr |
Worker version of Community Intervention. |
Yes |
| ARMHS Community Intervention TCL |
You provide Community Intervention as defined in this guide, to a recipient who is in an MA facility (hospital, residential treatment, nursing home. TCL stands for Transition to Community Living. Prior authorization from your supervisor before providing this service is required. |
Yes |
| ARMHS Community Intervention TCL by Worker |
Worker version of Community Intervention TCL. |
Yes |
| ARMHS Contact & Scheduling |
Recording efforts to contact individuals and schedule services. Use when contacting referral sources and members of the individual's extended support team also. |
No
|
| ARMHS File Note |
Putting brief notes/information in a recipient's file for the record. |
No |
| ARMHS Group |
Providing group services to three or more participants. Group services require prior authorization. Do not document group services if only 2 participants attend. Instead, Split the time between the two. |
Yes |
| ARMHS Individual |
Providing regular individual ARMHS. |
Yes |
| Progress Review in Session |
This service is an ADD-ON (like travel) to ARMHS Individual that indicates you completed a monthly progress review in a session where the bulk of the session was ARMHS Individual. |
No
|
| ARMHS Individual by Wkr |
Worker version of ARMHS Individual. |
Yes |
| ARMHS Service Coordination |
Service Coordination by a Practitioner or Worker. This includes coordinating with providers within Accend, and others, outside of the agency. |
No |
| ARMHS Transition to Community Living |
A very specific service to recipients who are in an MA facility (hospital, residential treatment, nursing home. Prior authorization from your supervisor and a Transition to Community Living Treatment Plan is required before providing this service is required. |
Yes |
| ARMHS Transition to Comm Living by Wkr |
Worker Version of Transition to Community Living. |
Yes |
| Clinical Support |
Clinical Professionals or Clinical Trainees providing support or consultation about the needs of an ARMHS recipient. |
No |
| FA Initial Interview or Observation |
Gathering information, in a face-to-face meeting with a recipient of ARMHS for the initial Functional Assessment and Status Assessment. This may be in an interview, or while observing them in activities while providing assistance. |
Yes |
| Functional Assessment Update Interview |
Gathering information, in a face-to-face meeting with a recipient of ARMHS for updates to the Functional Assessment and Status Assessment. |
Yes |
| Functional Assessment Writeup |
Writing the findings, while not with the recipient, of the interview for the initial or update Functional Assessment and Status Assessment. |
No |
| Treatment Planning Initial Interview |
Gathering information, in a face-to-face meeting with a recipient of ARMHS for the initial Treatment Plan. |
Yes |
| Treatment Planning Update Interview |
Gathering information, in a face-to-face meeting with a recipient of ARMHS for updates to the Treatment Plan, including conducting a Progress Review face-to-face with the individual. |
Yes |
| Treatment Planning Writeup |
Writing up the findings, while not with the recipient, of the Treatment Plan interview. (Complete as much as the write-up with clients as possible.) |
No |

Progress Review
Functional Assessment Update
Each update to the Functional Assessment, examines new strengths and resources an individual has obtained, and whether or not he or she has made progress in any of the following ways:
- has learned and is using new skills that have improved functioning;
has made changes in his or her living and social environments that will aid in recovery and promote stability;
- is using formal and informal supports more effectively;
- is managing health care needs, and using health care resources more effectively, reducing the impact of health on functioning;
- is learning symptom management/coping skills to avoid or reduce drug or alcohol abuse to reduce its impact on functioning; or
- is engaged in and using mental health and health care services effectively to achieve recovery goals.
Treatment Plan Progress Review
Complete all Progress Reviews with the people you serve, unless it is impossible because the individual has disengaged from services.
The Progress Review is due every 60 days and should describe what has happened (progress, or lack thereof, and significant events or breakthroughs that occurred during the month) sufficiently enough to serve as a brief summary of the progress notes written during the period reviewed.
Each review accumulates until the final Update or Discharge Review for each Treatment Plan. The review:
- examines progress toward goals and objectives,
- ask whether or not these remain the individual's goals and objectives,
- identifies new goals and objectives, or redefines and improves on current ones.
All of the above are indicators of progress toward recovery as defined by the individual. His or her goals, and recovery vision may change, or evolve, but the purpose of re-assessment and review is in part to identify these changes and respond with the goal of optimal functioning, stability and successful discharge.
Read about Progress Review now in Principles of Person-Centered Assessment and Planning in the Assessment and Planning section of this guide.

Begin With the End in Mind
Ultimate success in ARMHS is successful discharge, when an individual has accomplished his or her goals. Discharge planning for ARMHS begins on the first day of ARMHS, and continues throughout the process until a recipient has achieved his or her treatment goals and recovery vision.

Helpful Tips:
When actively preparing for discharge, we have often experienced an interesting phenomenon: individuals often report decompensation, an increase in symptoms or impairments in functioning, as ending services becomes imminent. Why is that?
There are many factors, but one to consider is this. Especially for those who have received services for longer periods of time, who is their support network? Does it extend beyond you, the supportive and unconditional person whom they have come to know and trust as they do you? Have you worked with them to build a formal and informal support network that will continue when ARMHS end? Do they have relationships with others like you, to whom they can turn for support when needed?
This is why we measure Support Networks as a core element of recovery. Consider this in your treatment, and discharge planning.
When discharge is appropriate depends on each individual, and his or her recovery goals.
For some individuals,
Disengagement
Sometimes, individuals choose to separate, or disengage from services, at times we perceive as premature or before they have accomplished all of the goals and objectives in the plan we have made with them. Why is this?
There are many reasons for this. Some factors to consider are these:
- Were the goals and objectives in the individual's plan his or hers, or were they ours? Did he or she have less ambitious goals that he or she achieved, and we missed this in our earnest and ambitious efforts to address all of the needs we saw and for which we wanted to offer help?
- Were our services meeting the individual's needs? Was our plan person-centered? Were our services responsive to the needs they identified each time we met with them?
- Were there needs and issues we missed, too focused on adhering to the plan we made some weeks or months ago?
- Did we "roll with resistance" or pressure them for more than they were capable of, or ready to take on, considering ambivalence and other factors?
- Have we been unconditional in our supports, or have we pressured them to achievement, fearful that failure would reflect poorly on our own performance?
Discharge Procedures
Discharge from ARMHS may occur in any of the following circumstances:
Administrative Discharge
Administrative Discharge occurs when a recipient has:
- Become irreparably and permanently uninsured for ARMHS services, and connected to service and support resources elsewhere
- Moved out of state
- Moved or been out of contact for a period of one month or more and contact is not possible because the client does not have a phone and we have no known address, or any collateral contact persons associated with the individual
- Moved to another county in the state where we do not have an ARMHS presence.
- Has been placed in an MA facility with a stay expected for longer than 180 days. Do not immediately discharge a recipient who moves to a treatment facility or short-term rehabilitation or nursing facility for fewer than 180 days. In this case, Consider developing a Plan for Transition to Community Living and offer these services.
- Chooses a service that is incompatible with ARMHS services (such as Assertive Community Treatment).
- Has been incarcerated and will remain so after any current assessment or treatment plan expires.
- Has transferred to ARMHS services with another provider.
- Is no longer eligible for ARMHS services for other administrative reasons.
Clinical Discharge
Clinical Discharge occurs when the recipient:
- Has achieved his or her goals/outcomes and reaches a level of psychiatric stability and status so that ARMHS services are no longer necessary, and has participated in a voluntary successful discharge process, including connections to formal and informal ongoing supports
- No longer qualifies based on a Diagnostic Assessment and Eligibility Screening using the eligibility requirements above during an recently-updated Diagnostic assessment that determines ARMHS services are no longer necessary, and has been informed of the finding, and received information about appeal rights.
- Has repeatedly declined to participate in assessment updates to maintain ongoing eligibility determination, with documented evidence of effort to schedule and conduct the session, including offering to provide the assessment at home as needed, arranging transportation, etc.
- Has needs that will be met better by another agency, and has been referred and admitted for ARMHS services with that provider.
- Asks to discharge. In this case another individual (Clincal Supervisor, another provider, Service Coorinator, etc.) should contact the client to obtain information about the reason for voluntary discharge.
- Has disengaged from services for a period of two months, with documented efforts to contact, schedule, re-engage and coordinate with other service providers within and outside the agency, or has indicated a desire to quit services. In this case, take the following steps prior to discharge:
- Someone other than the assigned ARMHS provider attempts to contact the individual investigate the reasons for disengagement.
- Make efforts to re-engage the recipient through other service providers or the referral source.
- If contact is lost after a period of one month, send a letter to the recipient's last known address, offering services and inviting the recipient to re-engage at any time, but providing one month to respond.
- Move the recipient to closing status for one month after inviting them to re-engage, planning discharge if no response within one month of the letter having been sent.
- After the date of planned discharge identified in the letter, complete a Discharge Progress Review and move the individual to Previous status.
ARMHS Provider Qualifications
Practitioner Qualifications
Education + Experience Qualifications
Education: Has completed at least 30 semester or 45 quarter hours in behavioral science or related fields.
Experience: At least 2,000 hours of experience in the delivery of services to adults or children with
- mental illness, substance use disorder, or emotional disturbance; or
- traumatic brain injury or developmental disabilities and completes training on mental illness, recovery from mental illness, mental health de-escalation techniques, co-occurring mental illness and substance abuse, and psychotropic medications and side effects.
Education Only Qualifications
Holds a master's or other graduate degree in the behavioral sciences or related fields; or
Has at least 30 semester hours or 45 quarter hours in behavioral sciences or related fields andbehavioral sciences or related fields and completes a practicum or internship that (1) requires direct interaction with adults or children served, and (2) is focused on behavioral sciences or related fields.
Experience-Only Qualifications
- Has at least 4,000 hours of experience in the delivery of services to adults or children with
- mental illness, substance use disorder, or emotional disturbance; or
- traumatic brain injury or developmental disabilities and completes training on mental illness, recovery from mental illness, mental health de-escalation techniques, co-occurring mental illness and substance abuse, and psychotropic medications and side effects.
- Has at least 2,000 hours of experience in the delivery of services to adults or children as described above, and receives Treatment Supervision as required by applicable statutes and rules at least once a week from a mental health professional until the requirement of 4,000 hours of supervised experience is met.
Graduate Internship Placement
Is a graduate student in one of the behavioral sciences or related fields and is formally assigned by an accredited college or university to an agency or facility for clinical training.
Alternatives for Persons Serving Non-English Speaking Populations
A Practitioner is fluent in the non-English language of the ethnic group to which at least 50 percent of the practitioner's clients belong, completes 40 hours of training in the delivery of services to adults with mental illness or children with emotional disturbance, and receives Treatment Supervision from a mental health professional at least once a week until the requirement of 2,000 hours of experience is met.
Mental Health Worker Qualifications
A mental health rehabilitation worker
- is at least 21 years of age;
- has a high school diploma or equivalent;
- has successfully completed 30 hours of training during the two years immediately prior to the date of hire, or before provision of direct services, in all of the following areas:
- recovery from mental illness,
- mental health de-escalation techniques,
- recipient rights,
- recipient-centered individual treatment planning,
- behavioral terminology,
- mental illness,
- co-occurring mental illness and substance abuse,
- psychotropic medications and side effects,
- functional assessment,
- local community resources,
- adult vulnerability,
- recipient confidentiality
- and, additionally,
- has 2,000 hours of work experience in the delivery of mental health services to adults with a serious mental illness, traumatic brain injury, substance use disorder, or developmental disability; or
- has a total of 15 semester hours or 23 quarter hours in behavioral sciences or related fields; or
- three years of personal life experience with serious mental illness; or
- three years of life experience as a primary caregiver to an adult with a serious mental illness, traumatic brain injury, substance use disorder, or developmental disability;
-
- or
- is fluent in the non-English language or competent in the culture of the ethnic group to which at least 20 percent of the mental health rehabilitation worker's clients belong, and
- receives during the first 2,000 hours of work, monthly documented individual Treatment Supervision by a mental health professional;
- has 18 hours of documented field supervision by a mental health professional or mental health practitioner during the first 160 hours of contact work with recipients, and at least six hours of field supervision quarterly during the following year;
- has review and cosignature of charting of recipient contacts during field supervision by a mental health professional or mental health practitioner; and
- has 15 hours of additional continuing education on mental health topics during the first year of employment and 15 hours during every additional year of employment.
Behavioral Sciences and Related Fields
Related fields are inconsistently defined in statutes, but these definitions include social work, psychology, sociology, community counseling, family social science, child development, child psychology, community mental health, addiction counseling, counseling and guidance, special education, nursing, occupational therapy, rehabilitation and vocational rehabilitation, and other fields as approved by the commissioner of the Department of Human Services.
Education in other fields must include 30 semester college credits in the following core class areas: human services, psychology, social work and rehabilitation with valid transcript demonstrating that the practitioner has the required qualifications.
Mental Health Practitioner Job Description
The focus of Adult Rehabilitative Mental Health Service is recovery. Mental Health Practitioners teach skills to develop and enhance psychiatric stability, social competencies, personal and emotional adjustment, and independent living and community skills, when these abilities are impaired by the symptoms of mental illness.
Core responsibilities of the mental health practitioner role are as follows:
Caseload Management
- Provide services at the frequency and duration identified in the treatment plan, or seeks clinical advice when the individual served indicates a need or preference for more or fewer services.
- Make and document at least weekly efforts to contact disengaged individuals and contacts at least one other provider (internally or externally) as a part of effort to find/engage them.
- Does assessment & planning and progress review work with individuals (documented as FA or Treatment Planning Interview) and never updates plans or assessments without recent contact.
- Meet or exceed all assessment and planning deadlines with exceptions for individuals who have disengaged in the weeks or months previous to updates.
- Proactively facilitate DA update interviews for all individuals at least one month previous to the due date.
- Proactively monitor individual's insurance eligibility renewal dates and takes action to prevent lapses in insurance.
Referral and Service Coordination
- Make and document referrals for all mental health services recommended in the DA, FA and other assessments, and documented individuals' preferences. Follow up when individuals decline.
- Identify barriers to participation in services, including, but not limited to maintaining stable housing, transportation, maintaining financial supports, etc. and advocates for necessary supports.
- Identify all mental health services to which current persons served have been referred, their current status for each, and level of engagement.
- Review the ICSP for individuals also receiving Case Management services and check for alignment of ARMHS Treatment Plan and ICSP.
- Document evidence of consultation with the Psychotherapist when developing the ARMHS Treatment Plan where applicable.
- Use custom time reports and check-in with individuals served to monitor engagement in other mental health services provided at Accend. Check-in with individuals on progress and satisfaction.
- Able to report generally on engagement and treatment progress in other services received by persons served.
- Where individuals disengage from other services, explore with them their reasons for disengagement and report back to the provider and supervisors.
- Maintain information in each individual's file on what other health care services they need at this time, referrals made, and participation, including well care and treatment for conditions.
- Maintain notes on other supports individuals need & referrals made to case management, housing, residential, vocational./educational, financial, legal, advocacy, and social services, etc.
- Document contact information for all providers of outside services, natural supports persons, referral sources & others who are part of individuals' recovery and extended support team.
- During each ARMHS Update Progress Review, examine and report on all of the above, including needs for services, referrals made, engagement and participation, and progress.
- Facilitate Recovery Team Meetings concurrent with DA updates, or participates in these meetings facilitated by others.
Treatment Progress
- Ensure each person served has shown measurable progress in at least one the 6 FA progress ratings in each of the domains identified as priorities for services/treatment since the last functional assessment.
- Ensure each person served has shown measurable progress toward identified goals or objectives (outcomes) in their current ARMHS Treatment Plan (or the previous plan if it has been recently updated.)
- Provide evidence that ARMHS services during the past year have resulted in at least one of the following positive outcomes for each person served:
- Improved psychiatric stability/symptom management
- Improved physical health
- Improved use of health care and mental health services
- Maintained or improved housing and/or independent living status
- Improved connection to formal and informal support networks
- Improved vocational, educational status or participation in other meaningful and purposeful activity
- Prevented or reduced mental health-related hospitalizations
- Prevented or reduced crisis team interventions or crisis placements
- Prevented or reduced need for residential treatment
- Prevented or reduced incarceration or other loss of independence such as mental health commitment
MHCP Manual: ARMHS
DHS Website: ARMHS
DHS Mental Health Policy Manual: ARMHS
This guide is a living document. We want to improve it with your help. Do you have questions? Found a typo? Find yourself wanting more information? Please send us your thoughts about anything in this chapter by tapping on the link below.
Updates to this Chapter
November 28, 2022: Level of Care assessment requirements updated to reflect new MHCP policy.
August 22, 2024:
Functional Assessment deadlines for updates clarified based on July 1, 2024 statutory changes (updates required every 365 days after the full Functional Assessment, where previously this was every 6 months).
September 30, 2024: Requirement for Notification of Adult Service Initiation to start ARMHS added here. This information did exist already in the Referral, Admission and Discharge guide.
November 8, 2020: Slight language change in DA requirements for admission.
December 18, 2024: Notification of Adult Service Initiation no longer required.