Overview
In this section, you will learn about documenting mental health services, including writing high quality progress notes, using electronic health records, and navigating the TabsTM electronic health records.
This section of the training guide was updated most recently on July 5, 2019.
Please note that Mental Health Travel Time, once found in this guide has moved to its own guide here, in the Services section.
Before you start here, please also read the Data Privacy and Security chapter of this guide.

What You Will Learn
Follow rules and guidelines for timely and concurrent documentation
Write high quality mental health services progress notes using TabsTM
Use objective language for recording observations in progress notes
You will document everything you do at Accend with a Progress Note. This includes...
- Direct services you provide
- Assessment, Planning, Service Coordination, and Documentation time and activities;
- Treatment and Administrative Supervision your receive;
- Training you receive;
- In and Out notes that list the time you started and ended each work day or shift; and
- Other work activities

Concurrent Documentation
Concurrent documentation means the following:
- Substantially drafting Progress Notes during the activity in which you are engaged, or the services you are providing, or immediately thereafter.
Drafting notes substantially means recording start/end times, and writing at least brief notes that describe the activity, observations, intervention, client response and plan as applicable.
- Completing and submitting Progress Notes for review and approval daily. Preferably submitting notes from each day by the end of each working day but not later than noon on your next work day.
- Correcting errors on notes that were returned to you and resubmitting by noon on your next work day.
There are times when documenting during direct services is not possible or appropriate. At these times, concurrent documentation means documenting as soon as possible after the service. These might include:
- When you are working with individuals for whom it would be disruptive or harmful to effective treatment to use electronic devices during direct services.
- When you are working with individuals who might cause damage to your electronic devices used for documentation.
- When you are providing services in a public space where you cannot assure privacy and security while documenting.
- When you have been specifically directed not to use electronic devices while deliverying specific services.
- Other times when your service activities prevent you from using electronic devices or documenting.
Why Concurrent Documentation?
Concurrent documentation assures these important elements of quality:
- Accuracy: Your progress notes are medical records. Your days at Accend are busy. Documenting concurrently using the guidelines above will help to ensure the accuracy of your records and prevent inaccurate records that could constitute fraud.
- Efficiency: Documenting concurrently also saves time. It is much easier to remember and record accurately and efficiently what you have done and observed if you write it down when it occurs, or within minutes afterwards, and before other events occur and cloud your memory. Trying to get all of the facts straight hours or days later takes much more time.
Fee-for-Service Billing
Most of the services that we provide are fee-for-service billed in units of time. We bill for the total number of units of services provided on a given day, determined by the total minutes of service provided, so your time records should be accurate to the minute.
Accurate record-keeping can only be assured by concurrent documentation. Do not round, estimate, or forget to change the start/end time for a scheduled service to reflect the actual time spent with each person you serve.
Objective Documentation
Objective documentation can be easily understood as this: document only what you can detect with the five senses: sight, sound, smell, taste and touch. Judgements, opinions, and conclusions have no place in objective documentation. This is a simple rule. Look at the examples below, taken from progress notes written by your colleagues to understand better how to apply it to specific situations. These are only a few examples. Pay attention to what you document and make sure it is objective.
| Example |
Why it is Incorrect |
Alternative |
| He was dressed appropriately. |
Applies a judgement as to what is appropriate dress.
May be unnecessary. |
Is it necessary even to describe someone's dress, unless it is out of the ordinary?
If yes, then you might write: "He was wearing a new suit and tie for his job interview this afternoon."
|
| She was upset, angry, frustrated... |
Unless she told you how she was feeling, describing and emotion is a conclusion. |
What specifically did she say? |
| He was depressed, anxious, manic... |
These are diagnoses, and only a Treatment professional may diagnose. |
What specifically did he say or do that appeared to be sign or symptom of depression, anxiety, etc. Did he cry or frown? Pace? Speak unusually fast or slow? Was he unusually quiet or unresponsive to questions? |
| She was cooperative and polite. |
Another judgement. |
She participated in the exercises and asked for help. She thanked me for my help. |
| He was intoxicated. |
A conclusion. |
His speech was slurred and he stumbled when he got up to walk toward the door. |
| He seemed, appeared... |
Whenever you use either of these terms, they are likely to be followed by an observation that is not objective. |
Do not use "seemed" or "appeared" as a way to include non-objective observations in your documentation. Instead, document what you saw and heard. If you are unsure, ask the person and document his or her response. |
Writing Good Progress Notes

Avoid Jargony Stuff and Rules that Ain't
You may have been trained in school or another setting to document in certain ways and might be surprised to hear that these rules do not apply at Accend. Here are a few examples:
- Referring to the persons you serve only as "client" in your notes We don't agree. Use their names, and pronouns. (Their name is right at the top of the page, by the way.)
- Referring to yourself or others by your job title. Also unnecessary here. Use "I" and "me" and the names of others. Include name and job title (or role or relationship to the individual) of others when it may not be clear to the unfamiliar reader.
- Use plain conversational language versus pretentiously formal language. "Stated" versus "said" is very common, for example. Most people just "say" things, they don't "state" them. "He told me..." is the plain language preference to "he stated..."
- Many people seem to believe that they must report on the individual's dress or appearance in every observation note. We often see "Dressed appropriately for weather and situation" in every observation. There is no need to report on dress unless it is out-of-the-ordinary (see guidance on Targeted and Relevant Observations below.

Keep Your Notes Targeted and Relevant
Observations are significant events, setbacks or breakthroughs, and out-of -the-ordinary circumstances. How a person was dressed, whether or not they arrived on time, and other such commonplace observations are not significant unless these are a significant departure from normal. If there is nothing significant to report in observations, it is acceptable to write: "Nothing remarkable."
In the Intervention and Response narratives of the note, describe the active treatment. It is not necessary to describe all of the details of interaction, as if recreating the entire session in the note. Include those details that are necessary to illustrate the specific mental health service intervention (active treatment) and how the individual responded.
In the Plan section be as specific as possible. When, where, you will meet next and what each of you will do between this session and the next are important details. Then, remember to follow up on plans made, and report on them, in the next session's notes.
Follow these best practices for writing high quality notes:
- Avoid jargon and confusing abbreviations. The acronyms for our services are ok to use, as are approved medical abbreviations by trained staff. Use other abbreviations with care so that your notes are clear.
- Use proper spelling, grammar and punctuation. If you struggle with this, trust your laptop's or device's suggestions for spelling, but take care not to let predictive text insert the wrong word! Other third party spelling and grammar apps (like Grammarly) are also very helpful.
- Take care when cutting and pasting, since special characters in some text software sometimes become nonsensical images when pasted into a browser-based system.
- Use the TabsTM clipboard when gathering information from one source to use in another. Its very useful and that is why we put it there!
- Write in simple, plain language. Don't assume that rules you learned elsewhere apply here. Ask if you're unsure, but we believe in plain language without pretense at Accend. Read the tips on the callout to the right for examples of what we mean by plain language.
Content of a Progress Note (Narrative)
Depending on the type of Progress Note you write, various elements will appear. These include narratives and data collection related to services and treatment. What follow is guidance for writing the narrative sections of notes. (Not all notes will include all of these narrative sections.)
Location and Location Description
You are asked to provide a briefLocation Description in these circumstances:
- When you schedule a service for someone else who is unfamiliar with the residence and may need special instructions, describe how to find a complicated address and/or access the building.
- When you provide services in Other Community Location: always describe that location, or locations.
- When you travel during services, describe the multiple locations to which you traveled.
- When you encounter difficulty in traveling to the location (road construction, finding the residence, or other) and your travel time or mileage is greater than would otherwise be expected.
- Other circumstances that you might find necessary to describe out-of-the-ordinary travel.
Location for InOut Notes
Location describes where you were for the duration of the shift. If you travel (between offices, between the office and client homes and other community locations for any portion of the shift, use Various Locations for the location of the INOUT note. It is not, in this case, necessary to use a location description because your other notes during the shift will explain that.
Risk Assessment
Risk assessment is for identifying any of the following that you observe while providing services. If you do not observe any of these, or any other risks not listed here, check the box that no risks were identified/observed and skip this narrative.
- Suicidal ideation
- Threats of or behavior indicating potential self harm
- Threats of or behavior indicating potential harm to others
- Threats to safety in current relationships, social and interpersonal risk, or behavior that may prompt harm from others
- Disorientation, wandering
- Substance abuse presenting imminent risk of harm to self
- Self neglect in basic needs, medication, personal care, etc.
- Risky behavior or impulsivity that could result in injury or illness, or financial loss (e.g. gambling, sexual encounters)
- Vulnerability to financial exploitation
- Unmanaged health problems presenting imminent risk
- Imminent risk of incarceration
- Current, or imminent risk of, unmet basic needs (housing, clothing, food, safety, health care)
- Imminent risk of loss of job or basic financial supports
- For children: credible threats to run away
- Other
Keep in mind the following all of the following when conducting a risk assessment, as well
If the risk represents an emergency:
Call 911, stay on the line until given permission to hang up and then call your supervisor for guidance.
If the risk you observe is a credible threat to others:
Contact your supervisor about threats of harm or violence to others made by your client and discuss the need to warn those threatened (Tarasoff Warning).
If you observe what may be abuse or neglect of a vulnerable adult or child:
Report abuse or neglect of children or vulnerable adults immediately using a Maltreatment Report and contact your supervisor for additional guidance on reporting.
Observations
Observations are targeted, relevant information about the specific individual to whom you are providing services. There is no standard observation reqiured or that you must include in this narrative. Some observations you might include are:
- The individual's reports of progress or actions taken on the plans made in previous sessions
- Good news reported by the individual
- Reported new current stressors, significant events or circumstances
- Targeted, relevant and objective observations that are out-of-the ordinary about the individual's:
- Appearance, presentation
- Household condition or circumstances
- Other out-of-the ordinary observations
Targeted and Relevant
Targeted and relevant means observations that directly relate to the client's status, mental health and functioning, and non-typical and ordinary behavior or appearance. Some examples:
- Jills's dress or appearance is disheveled, messy, unkempt when he is normally clean and neat.
- Jack is dressed in a new suit in preparation for a job interview later that afternoon, and this happens to be a goal you've been working toward.
- Jimmy comes to school without a coat in the winter.
- Jane has symptoms of, or reports, a serious injury or illness.
- Judy's attention and concentration is unusually scattered. She says she is "tired" and "did not sleep well last night." Judy usually sleeps well, so is out-of-the-ordinary. In your observations also explore why she was unable to sleep and record what she says.
Objective
Objective means observations that you see and hear and not opinions or judgements. Do not use expressions such as "seemed angry" or "appeared tired" to justify opinions or conclusions. Quoting the person (She said she felt "tired, anxiouis, worried, angry..") is an objective observation.
Note
The narrative Notes appear only on some types of progress notes. These are for describing the content of the session, activity, or information you want to record. For most direct treatment or services, you will instead describe Intervention, Response, and Plan.
Intervention
Intervention describes what you did. How you gathered or presented information, taught skills, intervened to help with a problem, redirected, responded to requests for help, etc. Provide information here relevant to the service or treatment. It is not necessary to describe every moment of the session, or detail of dialog or interaction. Provide a concise synopsis that illustrates that you provided the service.
This synopsis should describe active treatment, teaching, intervention, assessment, planning, progress review, and other activities that are consistent with the service provided.
Response
Provide a brief, objective synopsis of how the individual responded to the intervention.
Plan
Plans should identify what you will do, and what the individual will do (and when):
- In response to a need identified in the session
- To use or practice skills learned in the session
- To prepare for the next sesssion
- To coordinate services with others based on something discussed or discovered during the session
- Or other plans made with the individual during the session, including when and where you will meet next.
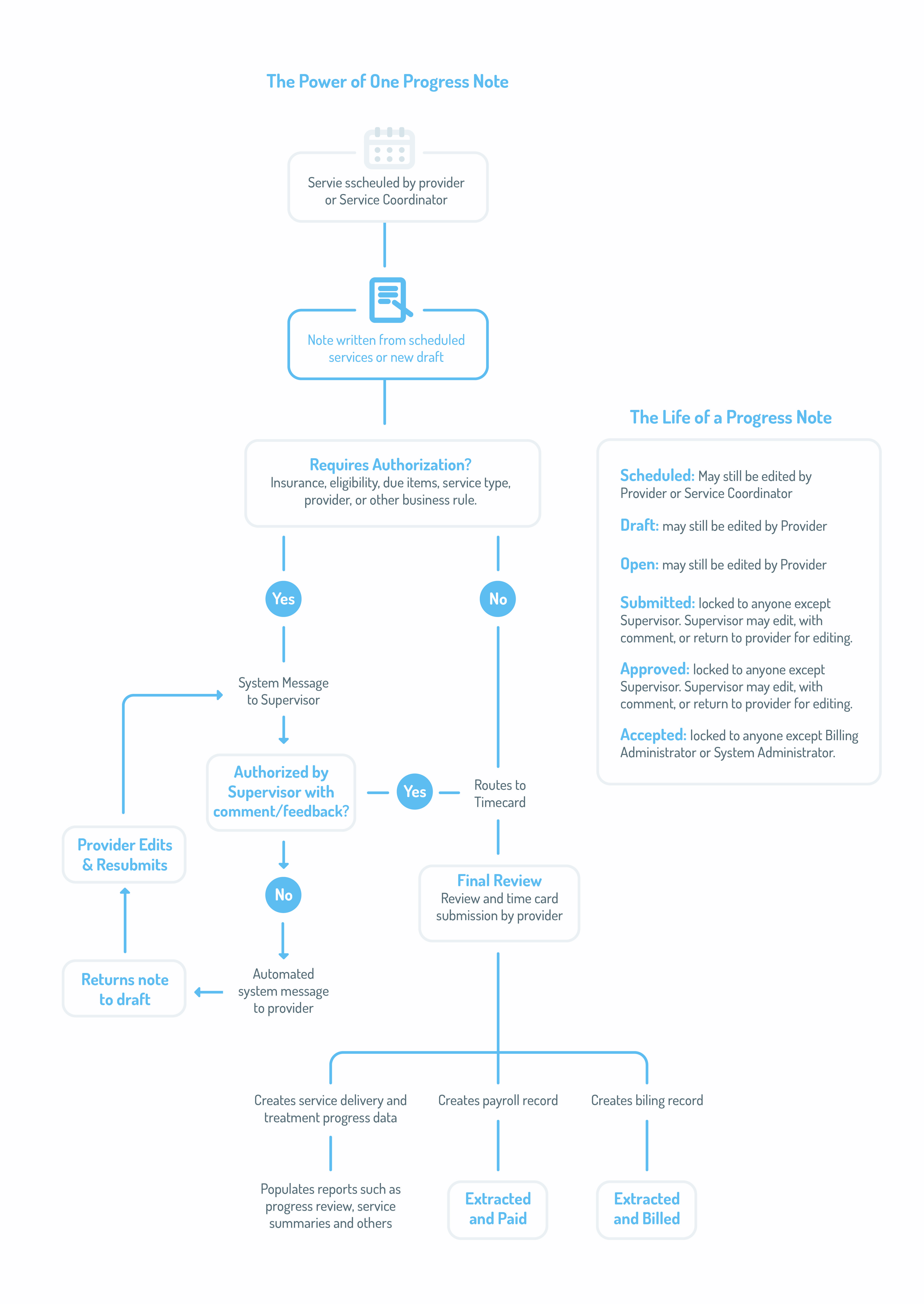
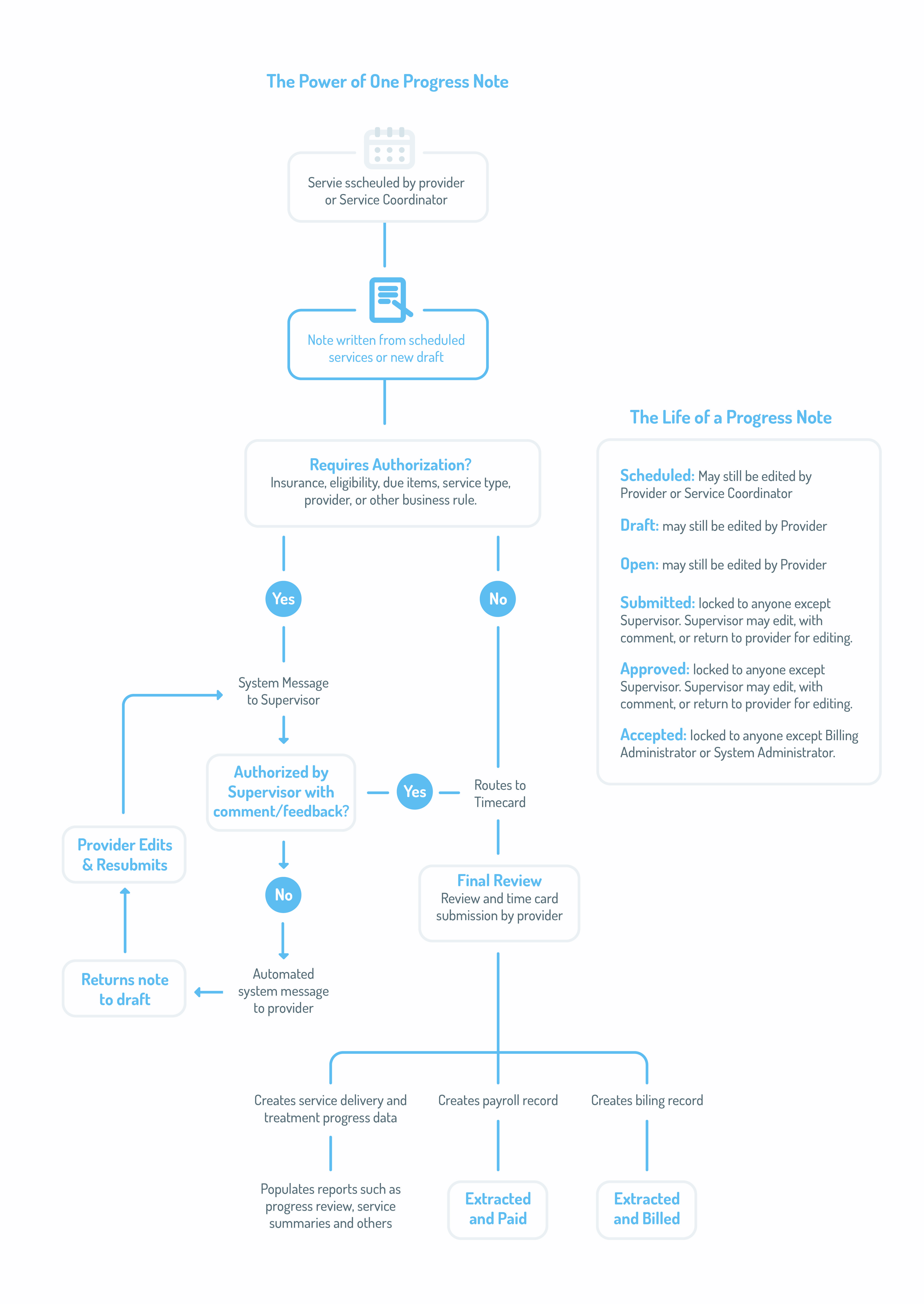
The Life of a Progress Note
When you write a progress note, you accomplish one or more of several several things automatically.
- Your outcome and progress data writes to the individual's Progress Review
- You create a billing record.
- You create a payroll (timecard) record.
- When authorization is required, and you choose an authorizer, TabsTM sends an automated system message to the authorizer to prompt them to review the note.
- For any direct service, your note creates a last seen date in that service category that you and others can use to monitor quality and engagement.
The diagram below shows the Life of a Progress Note.
For documenting travel, follow this link.
Document location as follows:
| Location
|
Use When
|
| Client Current Residence
|
Providing services to an individual exclusively in their own current place of residence, including temporary residences (e.g. hospital, nursing home, rehab or treatment facility). |
| Corporate Office - (Specific)
|
Activities or services provided for the entire shift in just one of our offices - select the office where you were located for the duration of the service/activity.
Do not select corporate office just because you started the day there, if later during the same shift (without a log-out) you traveled to see a client to provide services, or if you worked during the shift at more than one office. Instead, use "Various Locations" as the location and explain the various locations in the Location Description.
If you spend time in more than one corporate office during your INOUT shift without punching out, use Various Locations desscribed below. |
| Home Office
|
Activities or services provided while exclusively working from home.
Do not use this location for Telehealth services or Virtual Staff Meeings. See the description of those below. |
| None (PTO)
|
Choose this only for PTO or Unpaid Leave.
This should not be a required field for either type of these notes, but sometimes pops up (for example when you change the note type from another that did require location). |
| School
|
Choose this when the school where you were providing services is not specifically listed in the location dropdown list, and name the school in the location description.
|
| Telehealth
|
Use "Telethealth" for client services only as allowed by our Telehealth (Telemedicne) Policy.
Never use "Virtual Meeting" for services to clients. |
| Various Locations
|
Use various locations in these two circumstances:
For INOUT notes when you travel to various locations during your shift without punching out, including travel between offices.
For specific service notes when you travel with or on behalf of (BHH or CMGT) the client during an uninterrupted service.
Explain the various locations in the Location Description. |
| Virtual Staff Meeting
|
For all training, supervision, non-billable meetings about clients and any other non-billable service activities when you joining a staff-only meeting online.
Never use "Teleheath " for activities that are charactarized by meetings between staff that do not include a client. |
You will document your training, or your time training others under the service category Career Development. Use the following service types to document training:
| Service Type |
Activity |
Travel Allowed |
Special Instructions |
| Trainee Being Trained Internal |
You are being trained by others in a classroom or one-to-one setting. |
No |
Identify the meeting type as Classroom or One-to-One. |
| Trainee Being Tutored |
You are attending a tutoring session. |
No |
Identify the meeting type as Group or One-to-One |
| Trainee Shadowing Trainer |
You are observing a trainer who is providing a billable service. |
Yes |
This record requires you to identify the trainer you are observing and the person receiving services.
Travel time and mileage is allowed for this type of training. |
| Trainee Attending External Class |
You are attending a class or seminar provided externally. |
Yes |
This must be prior-authorized.
Travel time and mileage is allowed for this type of training.
Identify the type of training in the meeting type drop-down.
|
| Trainer Training Trainee |
You are the trainer. |
No |
Identify the meeting type as Classroom, Tutoring, or One-to-One |
Observation and Direction
(Formerly Trainer Observing Trainee) |
This is provided while the trainee is providing a service to an individual, or other competency return demonstration. |
Yes |
You must identify the person receiving the service and the trainee you observed.
Do not use this service type for EIDBI Observation and Direction.
Mileage is allowed to this type of training when it is provided out of the office. |
Documenting Internships
Non-Employees
Interns who are not employees should document their time as follows (using only the following note types):
Internship In&Out: to document time spent.
Client services: and client-associated note types such as File Notes, Service Coordination, work on client assessments, etc.
Treatment Supervision: using Treatment Supervised General (Career Development note types), or Treatment Supervised Client Specific (found in the category Clinical Professional).
Interns who are not employees do not need to use note types such as Timecard and Note-Writing, Client-Related Non-Billable time, Discretionary Non-Billable time, or any training. All internship activities are training. Decribe training activities within the In&Out note.
Employees Who are Interns
Interns who are employees may have assigned projects to meet internship learning activities, literature reviews, participation in community groups as learning experience, which are not paid work time and they should use Internship In&Out to document these activities.
For more information on internship documentation read the career development guide here.
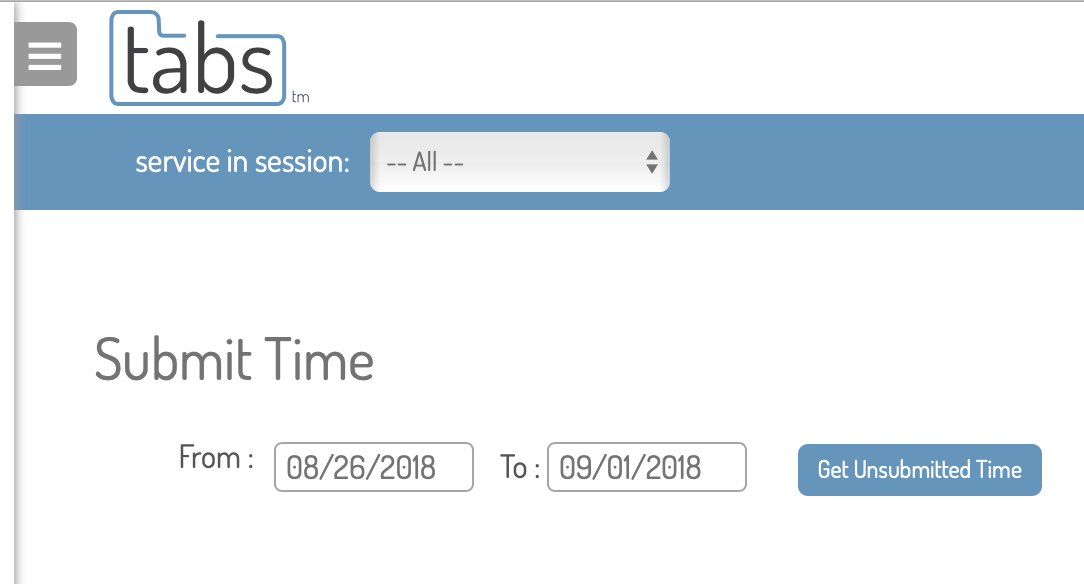
Submit Time Daily
Submit all time daily. This allows those who review and authorize time to do this throughout the week, and gives you time to make requested edits or corrections.
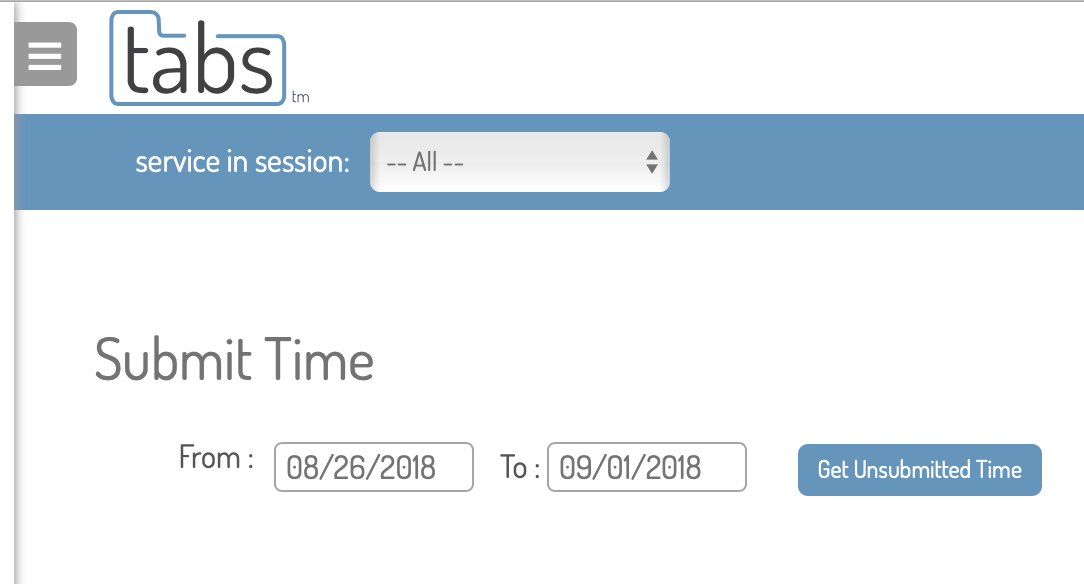
Submit All Time
When submitting your time, make sure you submit it all. TabsTM helps you with this. Look at the image to the left. Today is October 21, but when I tap on review and submit time, the date range 8/26/18 to 9/1/18 appears. This is because I have unsubmitted time from that week.
Do not ignore this and change the date range! Tap Get Unsubmitted Time to view your old time, and then repeat the process until you are current.
Read and Respond to Comments
When a supervisor comments on a note, TabsTM automatically notifies you. Check your messages regularly and make edits to the note as requested. When you do that, write your own response to the comment on the note, reporting what you did, or if the instructions are unclear, ask for clarification.

You may receive a lot of system messages. Use search function to narrow the list to what you're looking for. In the example here, I've found a message telling me someone has commented on a note I wrote.
You can use this search strategy to narrow your message list using any word, phrase or part of a word. Do this daily to keep up, and clean up your message box regularly by deleting read messages.

Schedule Repeating Appointments
The TabsTM scheduling tool is easy to use. We recommend that as much as possible, you arrange and schedule repeating appointments with the people you serve. This will make it easier for both of you to connect, and save you time in re-creating your schedule every week. To schedule repeating appointments:
- Navigate to home > my schedule
- Tap on the calendar where you want to set an appointment
- A dialog box will appear, with options for selecting client and service category
- Select these and tap Schedule Service
- The note will open and you can enter details (start, end, location, service type, etc.
- Check the box on the bottom labeled "Schedule Repeating Appointments"
- Choose from among the options for Max Date for Repeating, Interval, and Day of the Week.
- From there, you can preview the repeating dates, or save the scheduled appointments.
Scheduling Your Availability
To achieve our mission of responsiveness we need to know availability of team members who are able to take referrals. Make your availability known thusly:
- Check the box indicating you can take referrals when submitting your time.
- Go to your scheduler and create a new appointment at a time when you know you are available.
- In the client selector, choose Non-Client.
- When the specifics screen loads, select the service type: Open for Scheduling or Referral.
Deleting Recurring Scheduled Appointments
To delete recurring scheduled appointments:
- Go to: home>my schedule
- Select Advanced Search
- Select a date range
- Select: Client Appointments (if this is what you are wishing to delete)
- Select the client, Service Category, and (optionally) a Service
- Tap: Filter Appointments
- Scroll to the bottom, select all and delete.
Non-client recurring appointments can be deleted by filtering for those in the same way.
Note and Time Card Review, Authorization and Approval
Authorization of Notes
Note authorizations must be done by the appropriate supervisor. If a supervisor receives a request to authorize a note that should have been requested of someone else (as described below), comment on the note, send it back to draft, and redirect the author to request authorization of the correct person.
Time Card Reviewers who are not Administrative Supervisors should not authorize notes unless they have been delegated this authority by the Administrative Supervisor (and then for specific note types only) with the approval of the Treatment Director. Reviewers who are listed as authorizers without this authority should comment on the note and send it back for revision to request authorization of the correct supervisor.
Treatment Supervisors should authorize notes only when the specific reason for authorization is Clinical, or when they have prior-authorized the activity. These occurrences are limited. See also the instructions below for instances when dual authorization is needed on Clinical Trainee notes.
For new employees (Trainees during the orientation period) where the authorizer is Administrative Supervisor below, the Engagement Coordinator (Orientation Trainer) acts as Administrative Supervisor and should authorize the service.
When Notes Require Authorization for Compliance (Assessment and Planning) or Insurance
When a note requires authorization for compliance or insurance, it should contain a deascription in the narrative what action steps were taken to resolve the problem, or (in the Plan section) what plans (for specific action steps, with target dates) were made to resolve the problem.
Direct Services
| Activity/Reason for Authorization |
Who Should Authorize, Instructions to the Authorizers |
| Due Items |
The Administrative Supervisor
Follow these guidelines for authorizing services where there are compliance problems (Due Items):
Diagnostic Assessment: If the DA interview has taken place prior to the service, but the write-up is not complete, authorize the service unless the Diagnostician indicates that the results of the DA may indicate the recipient is no longer eligible.
Other Required Assessments or Treatment Plans (including signatures on plans): authorize the service only if the required element is completed and approved on the same day as the service.
If the overdue items are not resolved, decline to authorize the note. Send it back for revision to Client-Related Non-Billable time.
Check that the provider has taken or planned action to resolve the compliance problem and documented this in the Plan section of the note or elsewhere in narratives. |
| Duration |
The Administrative Supervisor
When the duration of the service:
- falls short of that required by the definition of the service, or
- exceeds the limit in the definition of the service, that recommended by our policies and procedures, or the maximum duration allowable by the payer,
Administrative Supervisors should comment and send notes back for revision if needed.
Notes that are too short in duration to meet the definition of the service must be deleted or revised to Client-Related Non-Billable Time.
Notes that exceed duration limits for the service must be revised with the balance (overage) documented as Client-Related Non-Billable Time. |
| Insurance |
The Administrative Supervisor
Follow these steps for authorizing services to uninsured individuals:
Mark the service as Commented, with a note asking the Time Card Approver to mark the service as Hold for Billing and Hold for Payroll before approving/accepting the time.
If insurance is re-instated and backdated to cover the service, the holds may be removed, and the service authorized.
Check that the provider has taken or planned action to resolve the insurance problem and documented this in the Plan section of the note or elsewhere in narratives. |
| Service Type: Case Management Being Mentored
|
The person (Case Manager or Qualified Treatment or Administrative Supervisor who did the mentoring)
This authorization is there for the mentor to assure that the mentoring took place as documented by the Associate being mentored.
Mentoring must take place face-to-face or by secure interactive video for the duration of the mentoring session while the person being mentored is providing Case Management services (including Assessment and Plannning writing.)
*Not all mentors can authorize mentoring notes at this time. That functionality will be added to Tabs soon. |
| Service Type: Clinical Trainee I EL Psychotherapy Notes
|
Treatment Supervisor
When there are additional reasons listed for authorization of a Clinical Trainee progress note, two authorizations are needed: Treatment and Administrative. Follow these procedures:
The Treatment Supervisor authorizes the note for Clinical reasons only.
The Administrative Supervisor authorizes the note when there are Administrative Authorizations needed (Due Items, Status, etc.)
The first of these to view and authorize the note should Comment on the note, noting their authorization of it, then mark the note and saving it as Commented (or send it back for revisions as needed).
When the comment is present from the colleague the second supervisor may authorize the note (or send it back for revision as needed).
|
| Service Type: ARMHS Community Intervention |
Administrative Supervisor
Review the note to assure that the service fits the definition of Community Intervention |
Service Type:
ARMHS Treatment Planning Writeup
FA Initial Interview or Observation or FA Update Interview or Observation
|
Administrative Supervisor
Treatment Planning Interview is limited to 4 sessions per calendar year. Functional Assessment Interview is limited to 6 sessions per calendar year. This means 2 and 3 sessions per Treatment Plan and FA respectively. When approving these service types, use a custom time report to monitor the frequency of these activities and impose limits. |
Service type:
Prior Authorized Info and Referral |
The Administrative Supervisor. This note should replace most of what was formerly "Case Management Outreach Face-to-Face" but must be prior-authorized. |
| Status |
Program or Office Manager/Service Coordinator for the Service Provided
Status authorizations most often appear on client notes when a client is not in Active or Initiating status when the service is documented. The role of the authorization by the Office Manager/Service Coordinator is to verify that a referral is moved to Active or Initiating status on the day of the first service, or other status issues are resolved. |
Non-Direct Services
| Activity/Reason for Authorization |
Who Should Authorize, Instructions to the Authorizers |
Service Type:
Other Prior-Authorized Time, or
Other Prior-Authorized Client Services |
The supervisor who prior-authorized the time or services.
Do not authorize unless prior authorization was requested (before the service was provided). When authorizing, make sure that the time spent does not significantly exceed the amount of time that was prior-authorized. |
| Service Type: Training Being Trained |
The Trainer, or
-the person who the trainer has requested to authorize, or
-if external training, the supervisor who authorized the external training.
When approving training time for employees past the orientation period, check their custom time report for training that has been previously authorized during the quarter. Team Members may complete training at any pace they wish. Paid training time is limited to 8 hours per calendar quarter, with exceptions where Accend authorizes a lengthy training.” |
| Service Type: other, not described above, or unclear |
Administrative Supervisor |
Time Card Approval
Content
Engagers (Orientation Trainers) should read most or all notes written by Trainees. Approvers should spot check notes for content quality in each element as defined in our Documentation Guide. Authorizers should use the opportunity when authorizing a note to review it for content as well.
| Section or Quality Element |
What To Look For |
| Overall Quality |
The note is written in person-centered plain language. The author of the note uses pronouns to refer to him/herself (not job title), the individuals name or pronouns to refer to the individual (not "client") and names and job title or relationship to refer to others.
All narratives written using respectful and objective language, including but not limited to:
- not describing emotions unless by the report of the individual,
- describing behavior using what the provider could observe with the 5 senses,
- not expresssing opinion or drawing conclusions.
|
| Risk Assessment |
Where risks are identified:
- Are they clearly and objectively described?
- Are actions taken and/or a clear plan made to mitigate the risk?
- If necessary, has a supervisor been contacted about the risk that was identified?
Where No Risks is checked: does anything else in the narrative indicate the presence of a risk that should have been described?
|
| Observations |
Observations should:
- Be targeted and relevant, meaningful and significant
- Provide information that is useful to understand the individual's status, progress since the last session, or impacts of behavior or presentation during the sesssion
- Report significant events that impact the individuals quality of life or treatment progress
- Be written objectively
|
| Intervention |
The intervention describes specific actions taken by the provider that:
- Describe active treatment (ARMHS, CTSS, EIDBI, Psychotherapy)
- Describe a meaningful core service (as defined by the Case Management and Behavioral Health Home guides)
- Provide additional useful informaiton (not simply regurgitate data provided in the data elements of the note).
|
| Response |
Describes the response of the individual directly relating to the intervention provided, potnentially including, but not limited to:
- objectively-described participaion and reaction,
- ability to demontrated the skill being taught,
- self-reported thoughts or feelings about the skill or the activities of session.
|
| Plan |
Includes but is not limited to potentially any of the following:
- What the individual will do between today and the next session (practice skills, take other actions);
What the provider will do between now and the next session;
- Any reporting the provider will do, or consultation he or she will seek based on what happened in the session or observations made during it - especially as regards risks identified;
- What actions the provider will take to resolve compliance or insurance issues identified in eligibility flags on the note.
- The date and time of the next appointmentt.
|
| Data elements (especially progress ratings) |
Is progress on outcome statements being recorded during the session?
Are other data elements required by the note type complete? |
Other Issues
Other issues Approvers should be on the lookout for:
| What to Look For |
Actions to Take |
Are services that require it authorized?
Was the correct person asked to authorize? |
Poke the authorizer if needed.
Notify both the selected authorizer and the writer of the note if the wrong authorized has been selected and provide corrective feedback, referring to this guide. |
| Are there services that require authorization are marked as Commented, with the comment: Hold for Billing and/or Payroll? |
Mark these services as Hold as noted in the comment, and then authorize and approve them. |
Does travel follow business rules from the guide?
-First/last travel of the day is the shorter of either the time/distance to/from home or primary office
-Travel between services is always to the next service, and there are no back to back from/to travel records without a service between them
-Travel time and mileage appears reasonable for the route
|
Open all notes with travel during service of over 10 miles. Spot check others.
Comment on and send notes back to draft where travel does not fit business rules and definitions in the guide. |
| When there is travel to or from the service (especially to first, from last service of the day) |
Spot check to see if staff are using the checkbox for "Was travel estimated?" and if yes, indicating the esimation method. This is required by DHS rules and was added to Tabs. First/last travel is always estimated, so this is a good indicator of a note to spot check. |
| When location is Other Community Location, Other Non Community, or Various Locations |
Check notes for the required Location description.
Location descriptions are not required for In and Out Notes when Various Locations is selected. This would be a common location for staff who see clients or commute between offices during a shift. |
When there is Travel During the service.
Assure that location is Various Locations and check notes for the detailed Location description either in the Location Dessription or the Narrative.
Does the location and narrative describe travel to a location that
- Would be naturally accessed by the individual on their own if the provider did not transport them there?
- Provides a natural and appropriate environment for treatment that is described in the note?
- Is not indicative of simple transportation services or errand-running?
- As appropriate for locations where treatment takes place regularly, does the provider eventually evolve toward meeting the indivudal there, rather than giving them a ride?
- Travel during service is reasonable, and fits definition of medically necessary travel during service in the guide
- When there is travel during a service, the location of service is Various Locations, and these are described in the Location text element in the note.
|
When travel during services does not meet with expectations described here,
- document your observations in a comment on the note that contains the problems,
- ark the note as "Commented", and
- bring this to the attention of the Administrative Supervisor by requesting they read the note
When a excessive travel during services is a pattern with a given provider, or when the travel is consistently not meeting the definitions and requirements for medically necessary travel during service in the guide, document this in Career Development using the service type Progress Notes Audit or Review Comments and bring it to the attention of the Administrative Supervisor.
|
| Other Issues to Watch for and Report |
When and How to Report |
Is time generally accounted for, for the majority of each shift, without long gaps.
Employees who do not need to gaps in time (unlesss requested as a part of a time study include:
- Supervisors, managers and administrators
- Administrative support staff unless asked to document in more detail
- EIDBI staff providing clinic-based services
- Highly productive staff in other services who are consistently meeting productivity requirements, and have received permission from their supervisor
- Any staff member who uses TimeTravel to concurrently document the majority of each work day
- Potentially more to come
|
When employees consistently have long gaps in documented time without meaningful activity, this may be worth investigating.
All staff in all positions should document all of the activities important for the client file and quality assurance, such as (but not limited to):
- Assessment and Planning Write-Up, and Prep Work
- Contact and Scheduling
- Service Coordination
- Advocacy on behalf of clients
- File notes that are important to the client record
- Other non-contact client work done on behalf of clients (especially in Case Managment in Behavioral Health Home where much of the work is done while not with clients)
Additionally, staff should document all Training, Treatment and Adminstrative supervision.
|
DISC and CRNB are not required for the positions listed above unless CRNB is important for a client file and there is no other appropriate service type.
Timecard and Notewriting is also not required for these positions, unless requested. |
Open as needed to see that these are being used correctly.
DISC (Discretionary Time) notes should never include client names or client-related activities
CRNB (Client-Related Non-Billable notes: check to make sure that the activity is not a billable/productive time activity.
Identify and report excessive, or patterns of repeated, use of either.
|
| Is time drafted concurrently and submitted daily? |
Report patterns of non-concurrent documentation to the team member's administrative supervisor by writing a note in the team member's file and inviting the supervisor to view it. |
| Documented INOUT time is far lesss than FTE and no PTO or unpaid leave is requested. |
Check for leave requests. Inquire with employee to see if they have forgotten to document some of their time. Follow up with supervisor if it appears there may be a problem. |
Providing and Documenting Feedback to Staff On Progress Notes
Provide feedback directly on notes using comments. Send them back as Draft if they need to be modified. Bring significant problems in a specific note to the attention of the Authorizer (if it is someone else) or the Administative or Treatment Supervisor as needed.
Document significant observations, problematic patterns or training opportunities in Progress Note writing in Career Development using the service type Progress Notes Audit or Review Comments and bring it to the attention of the Administrative Supervisor and Engager (Trainer) as applicable.
This documentation should include whether or not team members are documenting concurrenlty and patters of this should not be allowed to continue for any period of time. Make a note in the file and bring this to the attention of the administrative supervisor.
When a team member has an open performance intervention for any part of Progress Note writing, the Reviewer/Approver will be the primary source of information on progress correcting the problem.
Remember always to look for opportunities to record and document positive feedback and progress using the same methods.
 Audits of Telehealth Services
Audits of Telehealth Services
If you are providing telehealth services by telephone, an audit will include your phone records. To assure that you have a successful audit:
- use your work phone only
- in your location description, include the method of telehealth service delivery (telephone, Zoom, etc.)
- keep your client phone numbers up-to-date in tabs
- as always, document concurrently.
Why Do We Audit?
When developing policies, procedures and expectations for timeliness and accuracy of documentation, our primary goal is to have records we can rely on to bill for services accurately and pay staff accurately. Because both are important to us, we will implement internal auditing procedures effective immediately to help ensure that policies and procedures are being followed, and that work time, mileage and target time records are complete and accurate with no pay or billing opportunities missed.
To ensure accuracy, concurrent documentation requirements currently include that:
-
records are drafted in close time proximity to services provided;
-
records that are scheduled or drafted in advance are edited throughout each workday to assure accuracy;
-
start/end times are accurate to the minute;
-
estimated records (such as travel) closely match expected time and distance (mileage); and
-
notes are completed within 24 hours following provided services.
Internal audits will occur at regular intervals and may include spot checks or targeted examinations. Any employee may expect his or her records to be audited at any time. First level audits will look at whether or not you are following concurrent documentation policies. If an audit exposes that you may not be documenting concurrently, you will receive formal reminders, your records may be subject to a more in-depth audit, and you may face potential disciplinary actions if audits expose verifiably inaccurate records. In-depth audits will look for problems we have observed in the past that could indicate inaccuracies, including, but not limited to, the following examples:
| Problem |
Using |
| Concurrent documentation policies and procedures above not followed |
Time stamps collected by the database on when notes are scheduled, drafted, edited and completed |
| Records that are substantially drafted in advance of a service that do not show evidence of editing at the time of the service or shortly thereafter |
Time stamps collected by the database on when notes are scheduled, drafted, and edited and existing records of user interaction with the database |
| Interaction with the database during documented travel time |
Existing records of user interaction with the database |
| Interactions with the database during services documented for a client that are unrelated to that client’s services (such as documenting on one client while with another) |
Existing records of user interaction with the database |
| Documented work time not supported by system interaction of user |
Existing records of user interaction with the database |
| Extraordinarily long (or short) travel times or distances |
Online mapping of routes and travel times (while always taking into account potential traffic delays at certain times, or location notes indicating the reason for excessively long travel) |
| User location inconsistent with documented location during work time |
User IP address at login |
| Records that conflict with documentation by others |
Comparison with related records of other users |
| Missed opportunities for billable travel |
DHS rules regarding mental health travel time
|
We understand the burden of concurrent documentation during busy work days. We are committed to making this process as easy and painless as possible. In the fall of 2019, we will release the app version of Tabs(TM), called Tabs TimeTravel(TM). This simple version of this app will capture start/end times and mileage with one or two taps on your iPhone each time you start a new service or travel record. As envisioned, the app will also offer automatic mileage capture using the iPhone’s GPS.
Meanwhile, however, we ask that you double your efforts, if needed, for concurrent and accurate documentation, keeping in mind that inaccuracies in medical billing records, intentional or not, can constitute medicaid fraud, and put you and the entire agency, at risk.
From time to time, your notes will be audited. The purpose of audits are to assure that you are documenting correctly and accurately, including
- Documenting concurrently, as defined above
- Using correct service types for the services you are providing, and other work activities you are reporting
- Remaining compliant with assessment and service planning as you provide services
- Documenting all of your work time and expenses accurately, so that you are paid correctly
- Documenting all of your client services correctly, so that we are able to bill for the work that you do
- Documenting all billable service time and travel accurately and correctly, within state rules, to avoid unintentionally inaccurate, and potentially fraudulent, records
What do Audits Look Like?
Progress note audits take several forms:
Each Monday when your supervisor reviews the time you have submitted, this is a type of audit. You may receive notes back for editing, or you may receive TabsTM system messages that someone has commented on a note you have written.
Throughout the week, your supervisor, or other administrative staff may look at your notes and provide instant feedback by commenting on the note where there is a problem. The purpose of these efforts are to head off potential problems before you submit your time. Please read and respond to the system messages you receive when someone comments on your notes.
Finally, at intervals, you will receive full audit using your timecards and TabsTM user history. If there are no problems or the audit is generally good, we'll record the audit and make a note of it in your file. If there are substantial problems, someone may meet with you for coaching/tutoring to resolve the problems.
Remember
Keep this in mind about audits: better we find the errors and work with you to correct tem, than an external organization like an insurance company or the Center for Medicare and Medicaid Services finds them.

>>Tap here for a brief tour of TabsTM
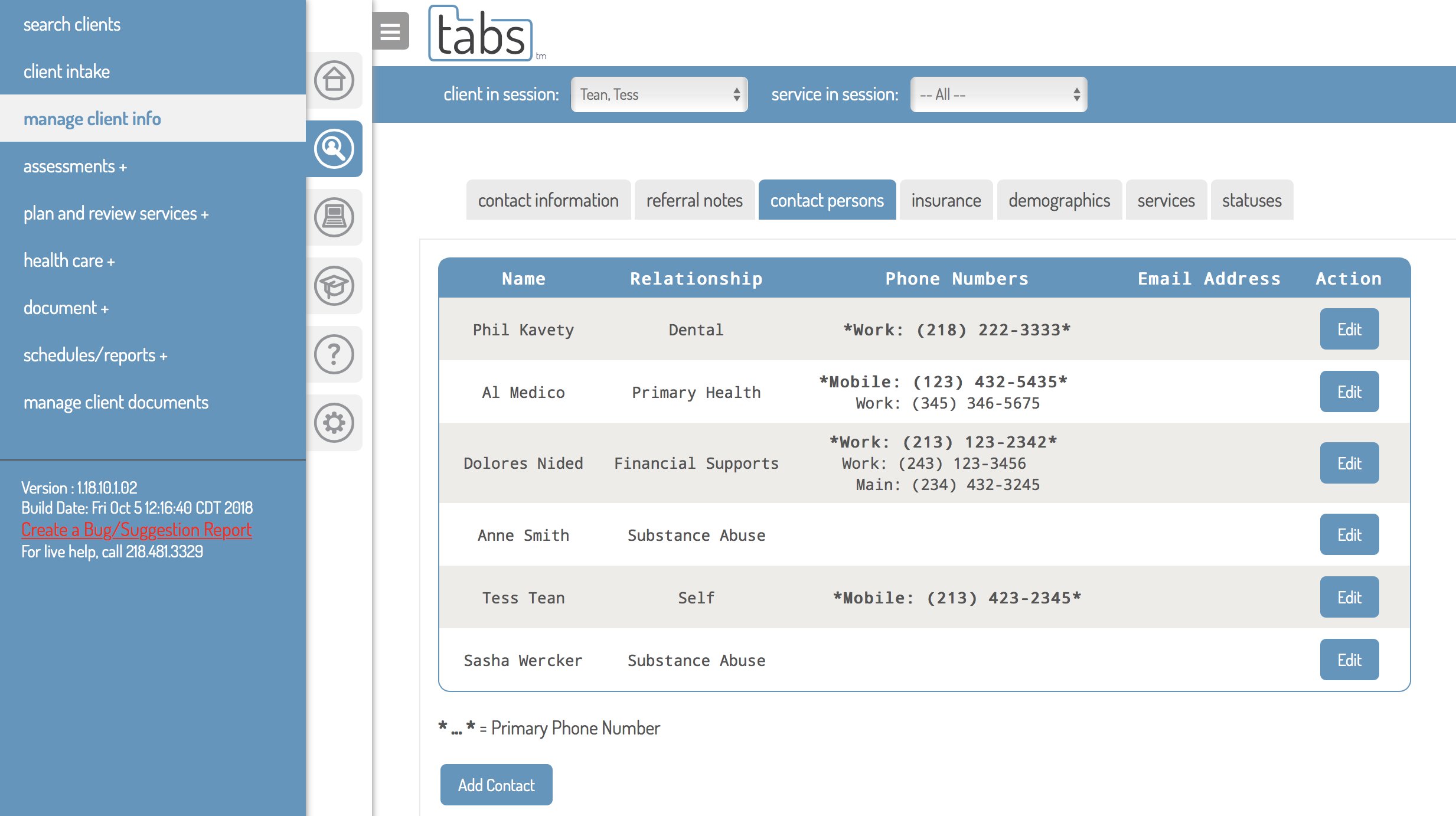
Tracking Collateral Contacts
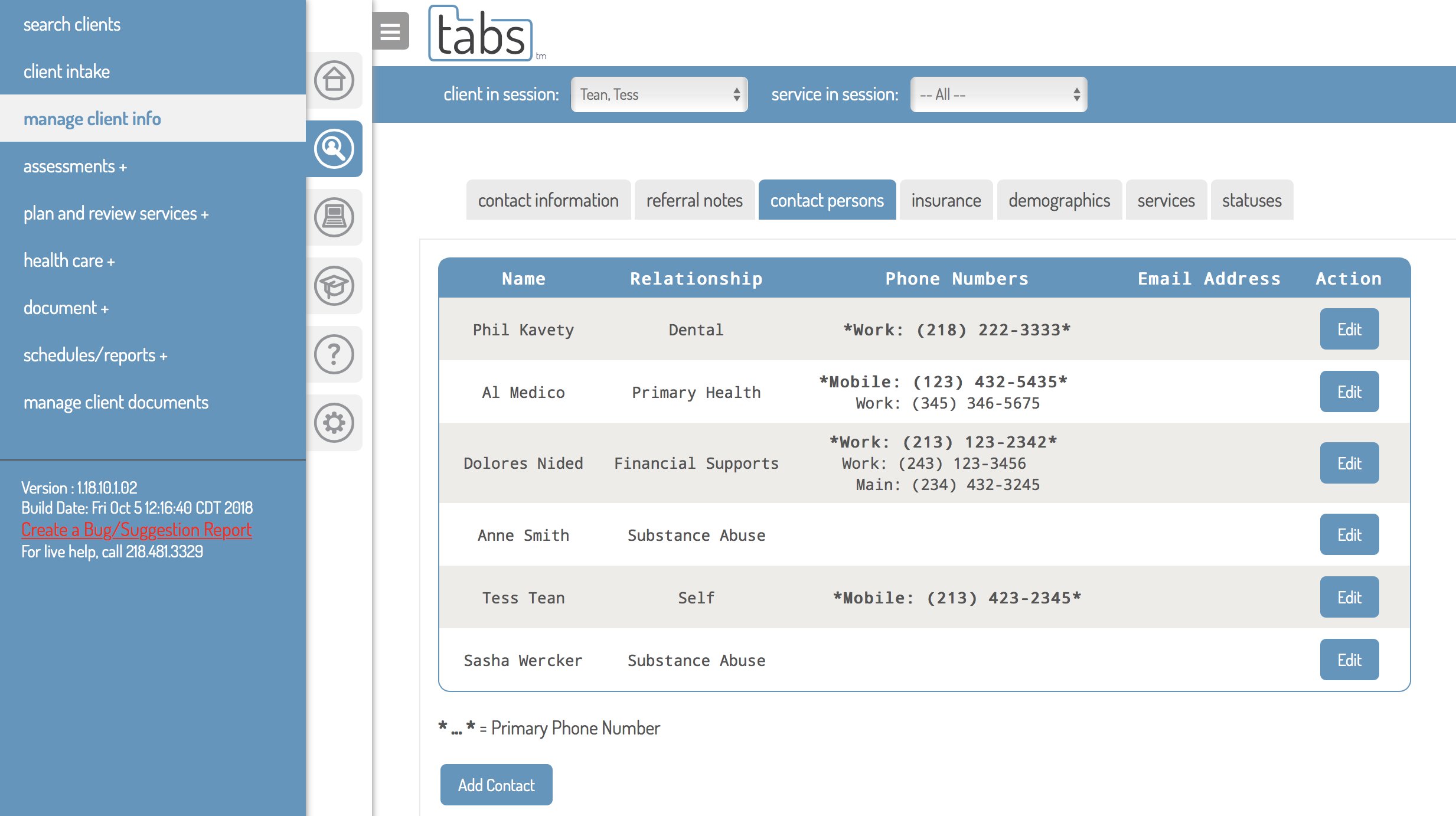

Collateral contacts refers to any and all key contact persons associated with a person served. Recording contact information for these individuals is important for services coordination and continuity. Add contact information for these key persons using the contacts tab in Client Information.
Tapping on this tab, you will see a list of all contacts currently recorded for the individual. If you do not see the person you're looking for, tap Add Contact to record their information. You may also use this utility for adding additional phone numbers for contact the individual served (for example the director of the housing program where a person lives, a common house number in a communal living setting, and other types of secondary contact numbers that may be useful in attempting to contact them.
After the form (shown on the right) for adding a contact person opens, fill out the form completely. Checking the box for "Is this a professional relationship" for example, will provide additional fields where you can enter additional information, including Agency, Job Title of the specific contact person, and a Case File Number if it exists, with that agency, for the person served.
Where the professional contact person is a health care provider, check this box, as this will facilitate future searches and queries in identifying health care professionals serving the people we serve at Accend.
When you learn that contact information has changed for these key persons, remember to keep contacts up-to-date.
Text Messages and Emails
Text Messages and Emails received by staff from clients, or sent to clients from staff are not part of the Health Care Record unless specific details of the communication are necesssary for the record. When this is the case, only the relevant portion of these communications should be included, by copying and pasting the text into a Progress Note of the type File Note, Contact and Scheduling, Insurance or Benefits Advocacy, Service Coordination, or other appropriate note types.
This should be done sparingly, while existing text messages and emails of this type should be deleted from phones, iPads and laptops at regular intervals.
Accend retains electronic health records that have been recorded in TabsTM in perpetuity. After 5 years from discharge, some records may be moved to an archived electronic storage, but will remain available to be retrieved as needed.
Other billing or health care records that are prepared outside of TabsTM are stored on secure servers for at least 7 years following discharge of adult clients and for at least 5 years following the 18th birthday of individuals who received services as a child.
If there are legal or other reasons that necessitate it, records may be kept longer than 7 years.
This guide is a living document. We want to improve it with your help. Do you have questions? Found a typo? Find yourself wanting more information? Please send us your thoughts about anything in this chapter by tapping on the link below.
Updates to This Guide
January 19, 2024: Text Messages and Emails
Guidance for Text Messages and Emails added, including when and how to include this communication in the health record, and encouragement to delete messages at regular intervals.






 Audits of Telehealth Services
Audits of Telehealth Services