What You Will Learn
Explain the purpose and goals of functional assessment
Explain the concepts and rationale for the domains in 6X6 Functional Assessment, and how they align with th SAMHSA Working Definiion of Recovery
The purpose and goal of the Functional Assessment process is to assess and identify functional strengths and impairments to:
- Help the individual articulate his or her recovery life vision or goal, service goals, needs and priorities
- Utilize the individual’s strengths of functioning and resources in any domain to build, restore and enhance functioning that is currently impaired in that same or another domain
- Formulate service planning based on the individual’s recovery vision or goal, service goals, priorities and best practice interventions
Along with the DA, the Functional Assessment is the core document used for identifying:
- Basic needs
- Current strengths and resources for acheiving goals and recovery vision
- Barriers to goals and recovery
- Current functioninng and impairments in functioning
- Links between mental health symptoms and impairments in functioning
- Strategies and priorities for mental health services and treatment
- Progress on all of the above (in subsequent FA updates)
The FA also serves to assess and identify functional strengths and impairments to:
- Demonstrate medical necessity and establish a “golden thread” documenting that necessity throughout the individual’s service record
- Guide the documentation for all services and interventions, and
- Justify reimbursement or payment for services
What is 6X6 Functional Assessment?
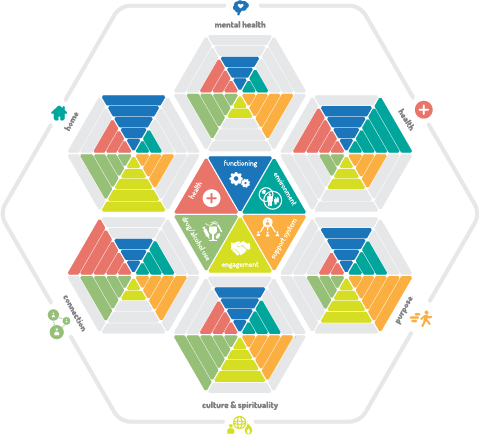
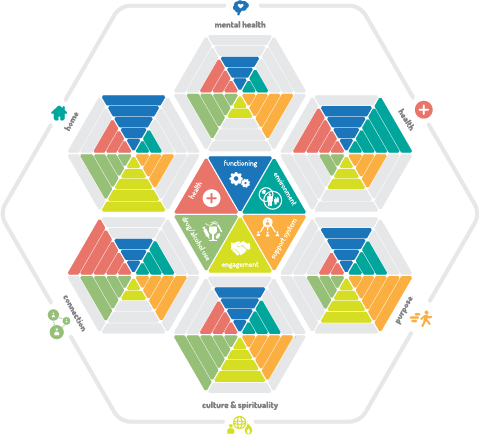
At Accend, we call our Functional Assessment the 6X6 FA. It is designed from the lessons we have learned in our many years providing adult mental health services, and around the SAMHSA definition of recovery you read about above. What is 6X6?
Since the beginning, the Functional Assessment for ARMHS and Case Management required assessment in 14 domains of functioning. We had two goals in developing the 6X6 FA. These were to:
- Simplify: shorten and reduce redundancy by
- combining related domains into a 6 larger categories, and
- focusing the assessment on what is useful
- Making the FA meaningful: creating data that can be used to
- guide treatment and
- measure progress in meaningful ways,
- related to a working definition of recovery
What follows are descriptions of those six broader categories and the sub-domains (domains from the original FA) included in them.
Six Domains of Recovery

1. Mental Health: While the SAMHSA definition defines mental health and health together as one of four elements of recovery, in our FA, we assess mental health symptom identification and management separately, while understanding the vital links between mental and physical health.
2. Health: Both impacted by and impacting mental health, physical health, including good health habits, nutrition, exercise, and obtaining and using health and dental care is a core element of recovery.

3. Home: The Home domain includes skills and resources for independent living, including activities of daily living, obtaining and maintaining housing, managing finances, and transportation.

4. Connection: Connection includes relationships with family, friends, neighbors, and effective interpersonal communication and self-advocacy skills with these, and with service and support professionals, landlords, and others.

5. Purpose: Purpose examines work, education and civic and community involvement. Important to understand is that purpose is defined differently for everyone, and can include many different "meaningful daily activities, such as a job, school volunteerism, family caretaking, or creative endeavors, and the independence, income, and resources to participate in society."

6. Culture and Spirituality: For some, culture and spirituality is an extension of Purpose. In their cultural and spiritual practices and beliefs, they find meaning and purpose. For some, culture and spirituality provides Connection to others and identity that grounds them. And for some, culture and spirituality informs Health care decisions, or is a core element of healing and recovery.
Finally, for some, culture and spiritual beliefs and practices from their past may complicate their recovery process as they redefine their belief systems or adapt to new or evolving cultural values or experience a process of social, psychological and cultural change through the blending of past and new cultural norms and values in a process called acculturation.
See the Advanced Guide: Integrating Culture and Spiritual Into Recovery, here.
Six Axes of Progress

What You Will Learn
Measure progress using 6 axes in the Functional Assessment
1. Functioning: Improving functioning where it is impaired by the symptoms of mental health is a core element of the community-based mental health services of Case Management and Adult Rehabilitative Mental Health Services. The 6X6 FA examines functioning in each domain and identifies how it is impacted by, or impacts mental health symptoms.
2. Environment: For some, impairments in functioning are a condition of an environment that is not safe, stable, or supportive. For others, where impairments in functioning are chronic, impacts of these impairments can be lessened, or accommodated by a supportive environment. In either case, rehabilitative services and case management can help individuals identify and make changes in their home, work, school and social environments that are supportive and optimal for them.
3. Support Network: An individual's Support Network includes natural, or informal supports like family, friends, neighbors, and community members, and paid professionals in health and mental health care, residential, vocational, educational, financial, social services and other fields. Assessing an individuals support network, and connecting individuals with support systems can for many, be a core and vital lelement of recovery.
4. Health: Where health conditions impact, or are impacted by, functioning or symptoms, assessment of these impacts, and treatment targeted at reducing either is another core element of recovery. And, where a health condition or physical disabillity is the primary cause of impairment in functioning, the case manager or rehabilitation practitioner can assess an individual's Environment and use of his or her Support Network and resources as a possible focus of treatment.
5. Substance Use: Substance Use can often be a form of self-medication, albeit one that is not conducive to recovery. Substance abuse or dependency can be a powerful barrier to recovery. Where abuse or dependency is a barrier, treatment might emphasize symptom management and healthy habits as an alternative to self-medicating with drugs or alcohol, and connecting with supports and resources to treat the abuse or dependency problem.
6. Engagement: Engagement measures an individuals readiness for change and participation in medically-necessary services and supports. It describes a persons progess moving from a place of ambivalence to partnering with providers and setting and accomplishing recovery goals.
Conducting the Functional Assesment

What You Will Learn
Conduct a Functional Assessment as a integrated part of treatment, not separate from it
Identify medical necessity for treatment in a domain
Conduct a meaningful update to a functional assessment using meaningful treatment progress probes
Write strong, person-centered and strengths-based rationale for treatment
Complete the Status assessment with each FA
Document assessment work using the correct service types
Rather than a one-time every 6-12 months event, Functional Assessment is an ongoing process. Rather than a compliance exercise and an interruption in services, the FA is integral to treatment, and one that provides benchmark measures of treatment success.
Dos and Don'ts In Functional Assessment
Do
- Begin with the end in mind: the individuals goals, and use the FA to identify strengths and resources for achieving them, and barriers/deficits.
- Complete the Functional Assessment with the individual, in a conversational and casual interview style, or while assisting with tasks and observing strengths, skills, and deficits.
- Familiarize yourself with the FA content so that you can gather information in this casual style.
- Consider (and describe the FA process to the people you serve) as a vital part of treatment, not a delay or interruption in providing services. Use FA updates to review progress, celebrate success, and indentify new needs and priorities.
- Begin the update immediately, as you gather information and observe or learn new information tht informs it.
Don't
- Conduct an FA interview in an inflexible checklist style, from beginning to end, rather allow the individual to lead where the discussion goes.
- Allow conducting the FA to delay response to immediate unmet needs. Rather, while responding to needs, gather information for the FA about what led to the current problem.
- Write a Functional Assessment when you have not had contact with the individual within the past month.
- Consider the FA (and describe it to the people you serve) a compliance exercise, or paperwork that delays or interrupts treatment.
- Wait until the deadline is looming to complete the FA. If you have not already begun gathering information, start work on the update at least a month before the deadline.
Identifying Medical Necessity for Treatment in Each Domain Selected for Treatment
For each domain where you will provide treatment or services, you will identify the reason why these services are medically necessary. Refer to the following descriptions for how to make a selection on this list item.
- Current symptoms impact functioning:
- Individual has lived independently for some time and has had opportunities to use or develop skills
- May have (but not necessarily) functioned better/more independently in this domain in the past.
- Current symptoms prevent optimal functioning at this time.
- Development was inhibited due to a history of symptoms:
- Typically applying to younger clients who have limited experience due to a history of severe symptoms, who may have lived at home with parents, or received other supports in the past to compensate for a lack of skills in this domain.
- Opportunities/experience were missed due to placements/behavioral health:
- Typically applying (although not in all cases) to younger clients who have limited opportunities to develop skills in this domain because they have lived primarily in structured/protected settings due to behavioral/mental health (hospitals, foster homes, treatment facilities) where opportunities were not available to develop these skills.
- Activities in this domain may be a trauma trigger:
- Past trauma associated with activities included in this domain causes the client to avoid necessary activities in this domain, or otherwise impairs functioning.
- When this is selected, describe how services will be coordinated with the client's psychotherapist to prevent further trauma by exposure to these activities without a deliberate plan or preparation.
- See the DA treatment recommendations for more guidance on this selection or consult with the diagnostician or therapist.
- Impaired functioning in this domain exacerbates symptoms:
- Impaired functioning in this domain is a contributing factor to increased mental health symptoms.
- (Recommended to be selected with others.)
- Impairments not linked to mental health symptoms:
- The client’s functioning is impaired as a result of physical disability, health, old age, or other reasons other than symptoms.
-
Writing Treatment Rationale
A core element in each domain selected for treatment in the FA is the rationale for treatment. The rationale written in the FA will populate into the treatment plan, in the rationale for each treatment objective. When writing rationale, keep these tips in mind:
- Write with the objective in mind
- Make the case for medical necessity
- Identify current strengths and resources as well as needs and deficits
- Identify what ARMHS or Case Management will do for the client
- Avoid the phrase “will benefit from…” in favor of "needs"
- For each Subdomain not recommended for Treatment, identify:
- What are the client's current strengths and resources that will contribute to/support treatment success in other subdomains in this section?
- What deficits in functioning or unmet needs can be addressed with treatment in other domains? How?
- For each Subdomain recommended for Treatment, identify:
- On what current strengths and resources can the client build?
- What are the client’s current needs, and deficits in functioning?
- How are deficits in functioning impacted by symptoms?
Making the FA Update Meaningful
As mentioned the FA is a meaningful foundation on which effective treatment is built. To make the FA Update meaningful, examine these probes:
- Has functioning improved?
- Has environment improved?
- Has support system grown?
- Have health impacts lessened?
- Have substance use impacts lessened?
- Has engagement in treatment increased?
- If none of the above, why not?
- Is continued treatment justified?
- If so, what will change moving forward?
- If not, what is the plan/recommendation?
Status Assessment
The Status Assessment is a brief survey of an individual's status in the following areas:
- Residential
- Employment
- Education
- Legal
- Family
Conduct a Status Asessment upon admission and every six months for persons receiving ARMHS and Case Management services. We are required to report the data we collect using this assessment to the state Mental Health Information System (or MHIS).
Adult Intakes
The Adult Intake Functional Assessment was designed to streamline the intake assessment process in order to move on quickly to Treatment Planning and services. Significant portions of it auto-populate from the DA for each domain. This, combined with a well-conducted intake interview before and after the intake Diagnostic Assessment means that the Intake FA can be nearly complete on that first day. It can certainly be completed and ready for approval following the first appointment for ARMHS or Case Management following the intake interview.
The Adult Intake Functional Assessment also contains all necessary elements for, and will eliminate the need to do additional assessments for any of the following:
- The Case Management Eligiblility Screening, if the individual has been referred for AMH-TCM, and
- The Behavioral Health Home Basic Needs Assessment, if the individual has been referred for BHH service.
Because the Adult Intake Functional Assessment is brief and does not contain all of the Axes of Progress contained in the full 6X6 Functional Assessment, it must be updated with a full 6X6 FA within 90 days of completion. This is also integral to the design: the Intake Functional Assessment identifies immediate, basic needs to promote responsive services, and allows for a more thoughtful and complete 6X6 FA done over time as the providers and individual build their relationship.
The Adult Intake Functional Assessment relies on an approved Intake Diagnostic Assessment to get all of the auto-populated content. The deadline for the DA is 7 days after the intake interview. Once the DA is approved, tap Refresh Assessment Data in the Intake FA to pull that information from the DA and complete the FA.
To us the Combined Intake Functional Assessment and Treatment/Service Plan, rather than opening an Adult Intake Functional Assessment, navigate instead to Service Plans. There you will find the Adult Intake Assessment and Plan. Use that document to create both the Intake Interview and FA, and the original Treatment Service. Plan. For more instructions on using this plan, go to Principles of Person-Centered Assessment and Planning, here.
The Re-Engagement Assessment and Plan
TheCombined Re-Engagement Functional Assessment and Treatment/Service Plan was designed to streamline the intake assessment process in order to move on quickly to Treatment Planning and services when a client re-engages with services after required assessments and plans have expired.
To us the Combined Re-Engagement Functional Assessment and Treatment/Service Plan, rather than starting a new FA or HWA, navigate instead to Service Plans. There you will find the Adult Re-Engagement Assessment and Plan. Use that document to create both the FA/HWA, and the ongoing Treatment Service. Plan. For instructions on using this plan, go to Principles of Person-Centered Assessment and Planning, here.
Record the Combined Assessment
After completing either of these documents, complete the brief Record of FA/HWA from Combined Assessment and Plan found in Functional Assessment to create a record of required following assessments potentially included in that document:
- Substance Abuse Screening
- CMGT Eligibility Screening
- Crisis and Relapse Prevention Plans
- Functional Assessment
- Health and Wellness Assessment
- Intake Interview
- Service Intensity Assessment
- Basic Needs Assessment
- Client Status Assessment
Check only those assessments that have been completed as a part of that combined document. This assessment and plan defaults to an expiration date of 3 months from approval.
Document Assessment Work
Use the following service type to document Functional Assessment Work
| Service Category |
Activity |
Use Service Type |
Additional Instructions |
| ARMHS |
All face-to-face interview and observation time for new referrals |
FA Initial Interview or Observation |
While helping with basic unmet needs, you will have an opportunity to observe and learn about what has led to unmet needs. Gather and document what you learn in the FA. |
| ARMHS |
Interview for updating the FA |
Functional Assessment Update Interview |
Your notes should reflect at least one Functional Assessment Update Interview for each update. |
| ARMHS |
Writing up either the initial FA update, not done with the individual |
Functional Assessment Writeup |
This is not a billable service. Only face-to-face or telehealth/telephone contact counts as billable time. |
| ARMHS |
Face-to-Face treatment planning, setting goals, for a new referral. |
Treatment Planning Initial Interview |
After completing the FA, begin immediately on this work. |
| ARMHS |
Face-to-face time reviewing progress on the Treatment Plan, setting new goals, identifying new objectives |
Treatment Planning Update Interview |
Progress Review should be a face-to-face service, not something done at a desk. |
| ARMHS |
Time spent not with the individual putting finishing touches the treatment plan or progress review while not with the client. |
ARMHS Plan or Progress Review Writeup |
Do as much of this work as possible with the people you serve. |
| Case Management |
Face-to-face time spent with individuals doing either assessment or planning |
xCase Mgt Assmt & Planning Face to Face |
There should always be several notes of this type prior to and in close proximit to assessment or plan updates. |
| Case Management |
Time spent not with the individual putting finishing touches the treatment plan or progress review while not with the client. |
CMGT Plan or Progress Review Writeup |
This is not a billable service. Only face-to-face or telehealth/telephone contact counts as billable time. |
| Behavioral Health Home Services |
Interviewing a BHH client for Assessment and Planning. |
xBHH Assessment and Planning Interview |
This is a face-to-face or telethealth service. |
| Behavioral Health Home Services |
Writing up the HWA and/or BHH Service Plan or Progress Review while not with the client. |
BBHH Plan or Progress Review Writeup |
This is not a billable service. Only face-to-face or telehealth/telephone contact counts as billable time. |
Guidance on Specific Sections
| Section |
Tips |
| Summary |
Besides summarizing strenghts, impairments, treatment recommendations, priorities for treatment domains, the Summary section also serves as a quality control section, prompting the author to keep the individual's entire record up-to-date. These prompts include such things as:
- Are key contacts recorded in the individual's file?
- Is the individual receiving all of the services that were recommended in the most recent Diagnostic Assessment?
- Are other services needed?
When reviewing the summary, check these and look for action items, goals and objectives written to connect the individual with needed services they might not be currently receiving.
Keep in mind the difference between recommendations and referrals. When an individual delines services, these might still be recommended by the assessment, even if referrals are not made.
|
| Basic Needs Assessment |
When reviewing the Basic Needs assessment, check these and look for action items, goals and objectives written to connect the individual with supports for unmet basic needs, if applicable. |
| Culture and Spirituality |
Culture and spirituality are more than just minority or not, and faith or religious beliefs.
The best cultural assessment explores the culture in which an individual lives and was raised regardless of race or belief system, family values, wealth or poverty, gender, gender identity, sexual preference, education, a history of acceptance or bias and so many other factors.
Lederach, J.P. (1995). Preparing for peace: Conflict transformation across cultures. Syracuse, NY: Syracuse University Press: "Culture is the shared knowledge and schemes created by a set of people for perceiving, interpreting, expressing, and responding to the social realities around them" (p. 9).
Spirituality can be found outside of religion, in the way one is motivated or inspired by nature, art, music, aesthetics, connections to others, personal value system and much more. Even a particular set of religious beliefs (or history of the same) and be comforting or dispiriting, affirming or constraining.
When reviewing this section look for and encourage a broad definition and exploration of each person's culture and spirituality.
|
| Mental Health |
Straightforward and the core of the assessment. It should inform all other sections/domains. Most importantly, assure the consistency of this section with all other sections/domains.
When an individual is receiving BHH services only, the Treatment Supervisor (in this case the Integration Specialist) should seek guidance from Mental Health Professionals where complex mental health conditions exist and services are not currently being provided to address them.
|
| Health |
A very important and complicated section, the Health section is key to integrated care. When reviewing this section, look for, among other things.
- Referrals for untreated medical conditions (diagnosis list).
- Action items, goals or objectives to address unmet health care needs, incliuding receiving preventative health and dental care.
Additionally, examine the diagnosis list for conditions that would have been short-term and may be resolved, but not expired.
When an individual is not receiving BHH services, the Treatment Supervisor, and complex medical issues are evident in the assessment, the MHP should seek guidance from the RN where these complex health conditions or diagnoses exist and services are not currently being provided to address them. We strongly recommend seeking consultation from nurses (RNs) in this section wherever complicated medical conditions are indicated, and always before approving plans that include goals and objectives for fitness, diet, weight loss, etc.
|
| Home |
A big section, including lots of things: housing, personal care and activities of daily living, safety at home, transportation,
etc. Most important here is making sure there are action items, goals, objectives for resolving problems that have been identified.
Where there are safety issues, check for immediate action plans to address this, or a complete Crisis Management/Risk Management Plan as applicable.
The treatment rationale here, if treatment is recommended, should identify specifically strengths in subdomains and deficits/needs in subdomains very specifically and describe both in the rationale for treatment.
|
| Connection |
This section focuses on interpersonal functioning, communication, immediate family, key other relationships, and safety in personal relationships.
Do not dismiss this section as it is vital. It is connection with others that aids more in recovery than anything else. Where can we help improve connections with family, friends and others?
This domain is not intended to describe relationships and professional supports from us or other providers. Where key relationships are limited to helping providers, this domain should be considered a high prority for treatment.
It is perhaps this domain where we can most improve our services by helping peope connect with others and bulld an natural support system that will help them sustain through, and after they have received, services. Review this section with those thoughts in mind.
|
| Purpose |
Purpose is more than just work or education. Purpose is closely related to Connection and should be reviewed simultaneously. Purpose can mean being a caregiving parent, or a caretaker to others, whether paid or unpaid.
Purpose can also mean civic or community involvement, volunteering, contributing to society in any way, or simply the activities in life that give one purpose, even online activity (the reason for getting out of bed each morning).
Review this section with other domains (especially Connection) in mind.
|
| Crisis or RMP |
This section should be reviewed keeping the mental health section in mind, as well as the risk checklist in the summary. If the brief plan is used for a person who has a history of risk or hospitalization, promote the use of motivational interviewing to encourage the individual to develop a more detailed plan.
When this section indicates that the indivdual wants to create a plan (or more detailed one), look for goals/objectives or action items planning this.
|
Updates
FA/HWA Updates are designed to be interpreted in in the context of previous assessments of the same type. If there are not significant changes, the template will not ask for a regurgitation of previous assessment information. A concise, economy of words is what we want. Sometimes, the previous assessment and current assessment need to be read/reviewed simultaneously for context.
What is most important to update in every FA is Treatment Rationale. This should take into account recent progress or decompensation. We always require fresh language here when treatment/services are recommended in any domain.
The WHODAS is the World Health Organization Disability Assessment Schedule, a generic assessment instrument developed by WHO to provide a standardized method for measuring health and disability across cultures.
The WHODAS is not a required assessment, but youmay be asked to complete a WHODAS in some cases to better inform treatment, especially for people with physical disabilities.
The WHODAS is a simple tool in which the individual responds as to the degree of difficulty they have experienced in the last 30 days accomplishing certain tasks or participating in certain activities. It is divided into 6 domains:
-
Domain 1: Cognition – Assesses communication and thinking activities; specific areas assessed include concentrating, remembering, problem solving, learning and communicating.
-
Domain 2: Mobility – Assesses activities such as standing, moving around inside the home, getting out of the home and walking a long distance.
-
Domain 3: Self-care – Assesses hygiene, dressing, eating and staying alone.
-
Domain 4: Getting along – Assesses interactions with other people and difficulties that might be encountered with this life domain due to a health condition; in this context, “other people” includes those known intimately or well (e.g. spouse or partner, family members or close friends) and those not known well (e.g. strangers).
-
Domain 5: Life activities – Assesses difficulty with day-to-day activities (i.e. those that people do on most days, including those associated with domestic responsibilities, leisure, work and school).
-
Domain 6: Participation – Assesses social dimensions, such as community activities; barriers and hindrances in the world around the respondent; and problems with other issues, such as maintaining personal dignity. The questions do not necessarily and solely refer to the ICF participation component as such, but also include various contextual (personal and environmental) factors affected by the health condition of the respondent.
The WHODAS may be conducted in one of three ways:
- By interview (our preferred method).
- Independently on paper (if preferred by the individual).
- By interview with a proxy (someone who knows an individual well when that person is not capable of participating). When using the proxy version, the proxy answers the questions based on their perception of the individua's difficulty with the tasks and activities described.
Tips for Conducting the WHODAS Interview
- Read the introductory phrase (e.g. "In the past 30 days, how much difficulty did you have in..." as often as necessary to make sure the individual is answering specifically for the past 30 days.
- If the individual asks for clarification read the guidance that accompanies each question. Do not intepret the question yourself.
- Encourage the respondent to answer the questions in regards to difficulties caused by health conditions (Health conditions (diseases, illnesses or other health problems, injuries, mental or emotional problems, problems with alcohol or drugs.
- If a respondent is prevented from doing an activity due to a health condition, rate the item as “5” for “Extreme or cannot do”.
- If a respondent has not experienced an activity in the past 30 days, but this is not due to a health condition, code the item as “N/A” for “Not applicable”.
Training for the WHODAS
To prepare for using the WHODAS, view the training video below courtesy of North Dakota Human Services, and then complete the WHODAS quiz in TabsTM.
The quiz is open book and guidance in the quiz references the portions of the WHODAS Manual found here:
Flashcards are used when conducting and interview. Laminated (reusable) flashcards and erasable markers are available from the office and can also be found here:
The 36-Question WHODAS Questionnaire for independent completion can be found here:
This guide is a living document. We want to improve it with your help. Do you have questions? Found a typo? Find yourself wanting more information? Please send us your thoughts about anything in this chapter by tapping on the link below.
Changes to this guide are listed below beginning in September 2022.
July 27, 2023
Document Assessment Work: service types for treatment/service plan and progress review writeup standardized.
September 9, 2022
Adult Intake and Re-Engagement FA/HWA and Treatment/Service Plan introduced and described.
September 27, 2022
LOCUS guidance removed and replaced with WHODAS guidance in the Level of Care (Service Intensity) Assessment section.
November 28, 2022
WHODAS guidance moved and described as a potential addition assessment that may be used in some situations. References to a required Level of Care (Service Intensity) assessment removed.